How does it work, and does conversational psychotherapy work at all
Hi, Habr! My
previous articles were mainly devoted to questions of pharmacology, but this is not really my topic, I am still a clinical psychologist (more recently), so today we will talk about conversational therapy in all its manifestations. tl; dr : in a long and tedious article addresses the issue of the effectiveness of psychotherapy ( yes, effective, within its limits of applicability, of course ), and also provides reflections on how this efficiency is achieved ( through the implementation of morphological and metabolic changes due to brain neuroplasticity ) .
At the end of the bonus for fans of video format (if there are any): record the presentation on the topic of this article: if you are lazy to read, you can see.
According to the definition adopted by the American Psychological Association, psychotherapy
For the purposes of this article, we will not draw a rigid distinction between psychotherapy proper and psychological counseling, which is defined as
In general, you already guessed , it will be about all forms of interaction between the specialist and the client (doctor and patient) when using word effects: from classical psychoanalysis to modern behavioral and cognitive-behavioral approaches. Or, to put it more simply, about " talking with a psychologist / psychotherapist ."
Indeed, we live in the 21st century, more and more sophisticated psychiatric drugs are offered to the market each year , intended to treat slightly less than all known mental disorders [3], and the relevance of psychological / psychotherapeutic influences is questioned by many.
However, there are reasons for using conversational (non-drug) methods.
First , they are in some cases just as effective as drug treatment: in the case of depression [4,5], panic disorder , social phobia [5] and even psychosis [6].
Secondly , in some cases they are more effective than drugs: in the treatment of OCD[5], some types of depression [8].
Thirdly , often the joint use of drugs and psychotherapeutic methods is more effective than only drug treatment [6,7,45].
Fourth , in some cases they have fewer side effects and are more easily tolerated [6].

Fig. 2 . Treatment with CPT and pharmacotherapy has led to a significant decrease in the activity of the tonsil in situations of anxiety. Source: [45]
Of course, I would not like the reader to get the wrong impression of psychotherapy as a panacea: in some cases, some methods of conversational influence are not only not useful, but also harmful (for example, “unstructured” types of psychotherapy when working with patients sufferingborderline personality disorder ) [9]. In the end, the measure of therapeutic effects determines the doctor in each case .
The attentive reader may note that this section is about psychotherapy, but not about psychological counseling.
Indeed, the latter has been studied much worse - both because of insufficiently developed research methodology ( how to evaluate the success of counseling during a divorce - not by the number of preserved marriages? ), And because of the much smaller prevalence of the principles of "evidence".
There are a great many types of psychotherapy [10]: cognitive , behavioral , cognitive-behavioral , rational-emotional-behavioral , narrative , psychodynamic , psychedelic , interpersonal , gestalt therapy , logotherapy , sensitization and processing by eye movement , etc.
Fig. 3 . From the Freudian associations [first level] to modern methods of therapy based on the principles of evidence.
And each school claims to be considered effective. And in some areas there is a completely imputed evidence base. At the same time, in most cases, explanations of this very efficiency are conducted through constructions adopted within the framework of this approach and are not quoted anywhere outside this framework.
So, for example, logotherapists believe that they achieve positive results by helping the patient find the meaning of life [11], supporters of the cognitive approach - by working with negative automatic thoughts [12], representatives of the psychodynamic direction - by working with the transference, drive and object relations [13], supporters of psychedelicthe approach is due to the work with perinatal matrices and systems of condensed experience [14] and etc.
At the same time, the majority of such explanations lose all convincingness as soon as they fall outside the context of the theory that generated them. So, for example, the cognitive postulate that thoughts affect emotions [12] is completely unacceptable within the psychodynamic school, where a completely opposite view is used.
Contrary to the opinion prevailing in the domestic environment, proven clinical efficacy ( to the extent consistent with the principles of evidence-based medicine , which is generally possible for psychotherapy) has not only cognitive-behavioral, but also, for example, psychodynamic therapy [15,16,17]. Those. different therapies based on completely different sets of axioms show comparable effectiveness.
Modern authors have noted [10, p. 7190] that all approaches to psychotherapy have a common base that ensures effectiveness:
One of the most interesting attempts to isolate and describe quantitatively the universal basis of successful therapy is the study of German authors [18], in which it was found that the predictor of the success of therapy is the difference in emotions that appear on the therapist’s face and those expressed by the client during the narration.
In other words, if during the first session a sad-faced client speaks about his pain (expressing " negative emotion"), and the therapist listens to him, demonstrating interest and satisfaction (" positive emotion "), the therapy is likely to be successful. If both express emotions of the same direction (" positive "/" negative "), then no.
The authors formally formalized the procedure testing, making a very limited “glossary” of emotions and selecting only those expressions of people that exactly matched him. As for determining the success of therapy (also not an easy task), we used therapist’s and patient’s estimates and objective indicators with symptom reduction.
Their conclusions are quite different from the predictions and explanations that psychotherapists themselves give - they talk about anything: about motivational readiness, about the radical of the client’s personality, about the level of organization of that person, about the deep patterns - but not about those emotions they express with their faces.
Such studies make us somewhat skeptical about the supposed mechanisms for realizing beneficial changes that psychotherapists / psychologists are talking about, and are pushing to find some more convincing ways to explain the existence of these very changes.
Some time ago, there was no way to objectively evaluate the effect of therapy on the brain, so psychotherapists made the most courageous (and often incorrect) assumptions about the presence and nature of such an effect.
Naturally, this situation could not last forever, and as soon as researchers had available methods for imaging the brain ( PET , MRI , fMRI , SPECT ), studies were published that aimed to determine the extent of the impact (or lack thereof) of conversational therapy on the physiological substrate of the brain .
Identifying this influence would solve several important problems - from the proof that conversational therapy works in general, to understand how it works, whether there is a difference between different types of therapy, etc.
Below is my attempt to systematize the data on the visualization of changes caused in the brain by speaking therapy.
It does not claim to be universal, but when it was created, I tried to include more or less sane studies and recheck the conclusions of the authors.
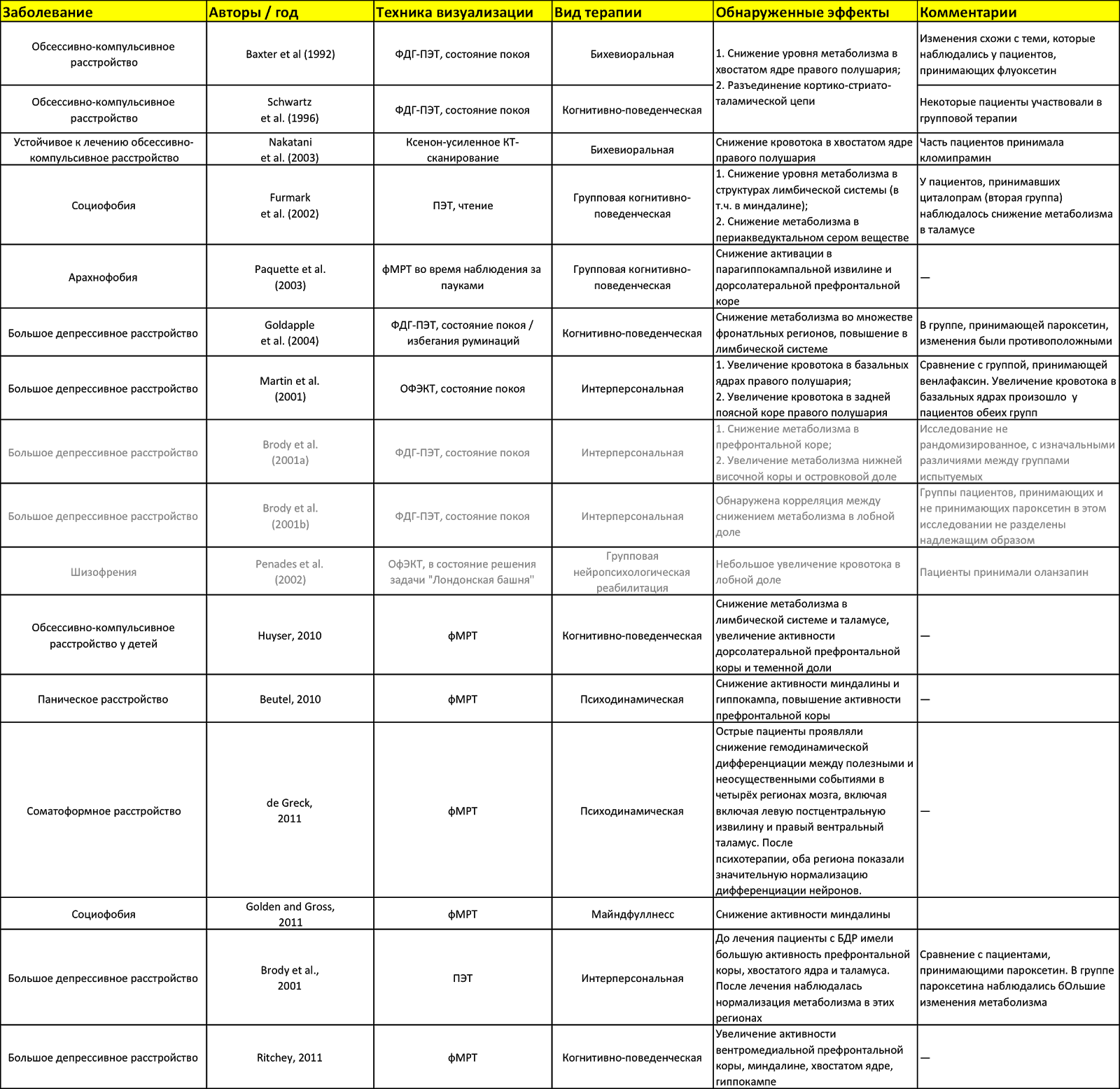
Fig. 4 . The effect of speaking therapy on the brain. Sources: [10, 32, 33, 34]. The table is available in Google Docs .
What do we see in this table? The first thing that catches your eye is the fact that the same areas of the brain (for example, the caudate nucleus or the amygdala) are affected by completely different types of therapy.
The second- this is what in some studies the activity of certain areas increases (for example, the amygdala in the Ritchey study), and in others, with the same therapy, it decreases (the limbic system, including the amygdala, in the study of Goldapple).
The third is that some studies are marked in gray. These are those whose design caused me the greatest doubts. But since today there are not so many such studies at all, I included them here.
What is the result? Visible some inconsistency data. It is caused by the fact that, firstly, the brain is a complex and controversial thing (I seem to have already spoken about this), and, secondly, by the fact that the research did not have a completely identical methodology.
What is the value of this table, if you can not directly compare different methods of PT? It is possible to make sure that conversational therapy “ does something with the brain there ”, and also that you can try to build some cautious conjectures on how this conversational therapy works.
But first, let's try to still highlight some patterns in these changes. To do this, we will not peer into the table for a long time, but use the data from the finished meta-analyzes.
It is assumed that with depression, CPT enhances cortical control on the part of the prefrontal cortex (especially its dorsolateral part), which inhibits (inhibits) impulses of subcortical structures [32, p. 6].
What this means: impulses that rise “ from the depths of the unconscious ” (this is just a beautiful metaphor) begin to be better controlled by structures that are more related to rational thinking.
If we recall how KPT works - namely, it is trying to replace “ automatic thoughts filled with cognitive distortions with more sober and rationalistic assessments of the situation ”, then we can trace some logic in this whole thing.
Therapy aimed at activating behavior presumably leads to the activation of the striatum and the activation of the reward system, including regions of the dorsolateral prefrontal and orbitofrontal cortex [32, p. 6]
What does this mean: again, the activation of “ more conscious structures ” as well as responsible for the behavior (as a set of motor, ie physical actions).
It is logical: we activated the behavior, activated the structures that are responsible for it. Since this therapy is essentially behaviorism, it is not surprising that the structures responsible are inclusive, incl. for reflexes and analysis of encouragement / punishment.
Overcoming repressed emotions and weakening unconscious guilt, which are important componentspsychodynamic therapy is presumably associated with a decrease in the activity of the subgenual anterior cingulate cortex [32, p. 6].
Everything is quite interesting here, since this very subgenual PPK is involved, including in overcoming feelings of fear (here you can draw far-reaching conclusions that, perhaps, psychodynamics are right, and the repressed guilt is therefore supplanted, because the psyche is “afraid” to accept it, but this will lead us away to speculations).
It should be noted that these assumptions appeared not from scratch, but on the basis of other studies (there are links in [32] on the corresponding pages).
Before discussing the results of research on the effect of colloquial therapy on the brain, you need to at least talk a little about how it works and consider some of its components that are directly related to the subject of the article in order to understand what the researchers have been doing there.
The main thing that can be said about the brain: it is complex . There are only so many ways to consider it that an unprepared person has a head in a circle — all these columns , departments , cortical maps , functional blocks , Brodmann fields , etc.
Fig. 5 . The progress of psychiatry and neuroscience through the eyes of the inhabitant.
We will not try here to examine the structure of the brain from all possible points of view, but only fragmentarily describe those parts of it that are relevant to the subject of this article.
It should be noted that the brain is a distributed system with a high degree of parallelism [21, p. 132], therefore, to say that one or another part of it performs a specific limited function would not be completely wrong. That is why all phrases like (“the amygdala is responsible for fear reactions ” should be taken as more or less successful analogies / metaphors, nothing more).
However, to some extent its components are specialized, and we will try to consider this specialization in the context we are interested in.
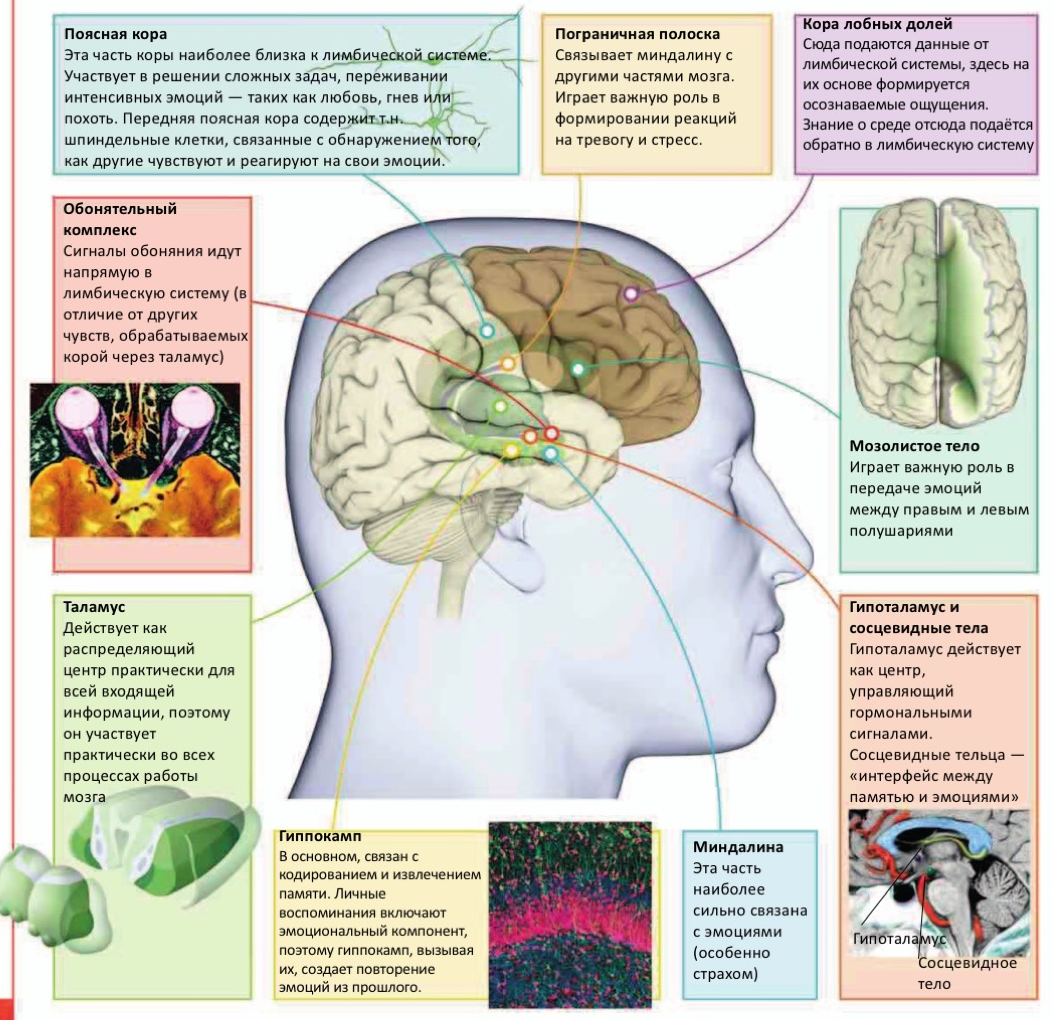
Fig. 6. Some components of the brain relevant to the subject of this article [31, p. 126].
The amygdala, it is also the "almond-shaped body." Located in the temporal lobe (median temporal lobe) [19, p. 232]. Since we have two hemispheres and two temporal lobes, respectively, are also two, then the amygdala is “divided into two pieces”. [19, p. 211]. This, by the way, applies not only to the amygdala.
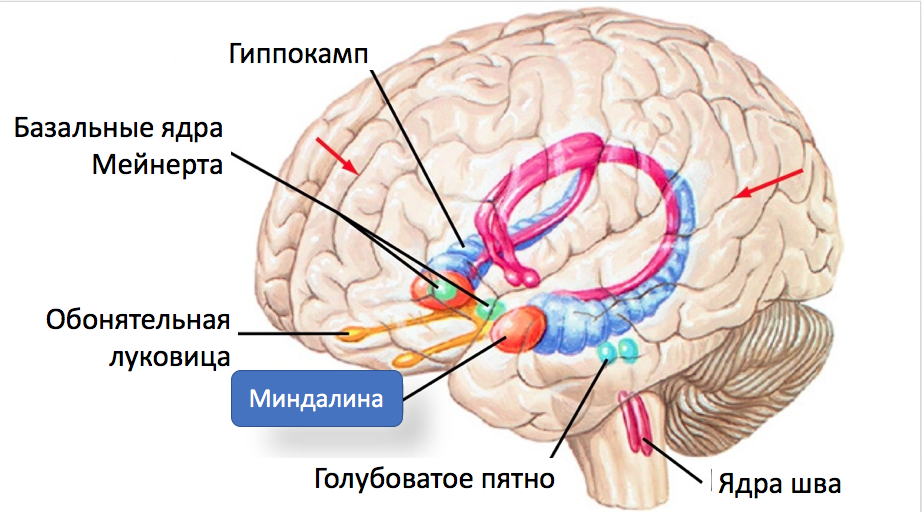
Fig. 7 . Tonsil and some of her connections.
Connecting with the prefrontal and temporal cortex , as well as with the spindle-shaped gyrus of the amygdala, plays a significant role in social and emotional cognition [10, p. 240] and is considered the main center for processing emotional information [19, p. 482].
Equally important is the fact that the amygdala is connected to the hippocampus[19, p. 216], which is involved in memorizing information (memory consolidation from short-term to long-term), its processing and retrieval from memory [19, p. 78].
The amygdala is part of the so-called. limbic sistama. It is shown that the structures of the limbic system and the nucleus accumbens participate in the “final calculation of remuneration”, assigning characteristics of pleasure or displeasure to the affective experience, and the warning / arousal system uses the reticular formation , thalamus, amygdala and cortex to assign personal experience and significance to this experience [ 10, p. 7186].
Studies have shown that the amygdala responds to emotional stimuli [19, p. 297] and mediates the conditioned-reflex reaction of fear [19, p. 538].
The dynamic interactions between the amygdala and the medial prefrontal cortex (mPFC) are conceptualized as a system that allows us to automatically respond to biologically significant stimuli, and also to regulate these reactions when the situation requires it [20, p. 113].
The amygdala has two “inputs” through which it receives sensory information. First, data comes from the senses to the thalamus , then they follow one of two independent paths: either directly to the amygdala, or first pass through the prefrontal cortex , and then reach the amygdala through the anterior cingulate cortex.[22, p. 19]:

Pic. 8 . Two modes of activation of the tonsils.
The first path is “ quick and dirty ” - the amygdala receives information that some kind of tin is created in the outside world, and does not go into details of what exactly this stimulus was: it starts to act, without taking time to figure out in a situation.
The second way is slower, but involves some analysis of incoming information. Data is processed in the prefrontal cortex.which integrates sensory information from the senses with information about the context of this stimulus received from the hippocampus, compares it with the experience stored in long-term memory, analyzes the previous similar situations and decides how real the danger is. She sends this decision to the amygdala, which, in the case of a positive response, triggers the preparation of the organism for the “flight or attack” reaction.
If the cortex " recognized the stimulus as harmless, " the amygdala on the contrary inhibits the stress response [22, p. 19].
For example, if an unprepared person noticed a snake in his path, it is highly likely that his amygdala will be activated by the thalamus without the participation of the cortex. At the same time, if it is a gerpentologist who understands that the snake is not dangerous, then, quite possibly, his reaction will follow the second scenario.
It has been shown [10, p. 7184] that the activity of the amygdala is elevated in depression and post-traumatic disorders . The situation is even worse if an increase in the activity of the amygdala is combined with a decrease in the activity of the prefrontal cortex.
Those. It is beneficial for us to reduce the activity of the amygdala, either directly or indirectly, through increased activity in the prefrontal cortex (see above data on the corresponding changes as a result of psychotherapy).
The caudate nucleus (along with the shell-core, which together form the neostriatum ) are part of the basal ganglia , which are connected by afferent (sensory, "incoming") and efferent (motor, "outgoing") connections with the structures of the midbrain - the black substance and subtalamic nucleus .
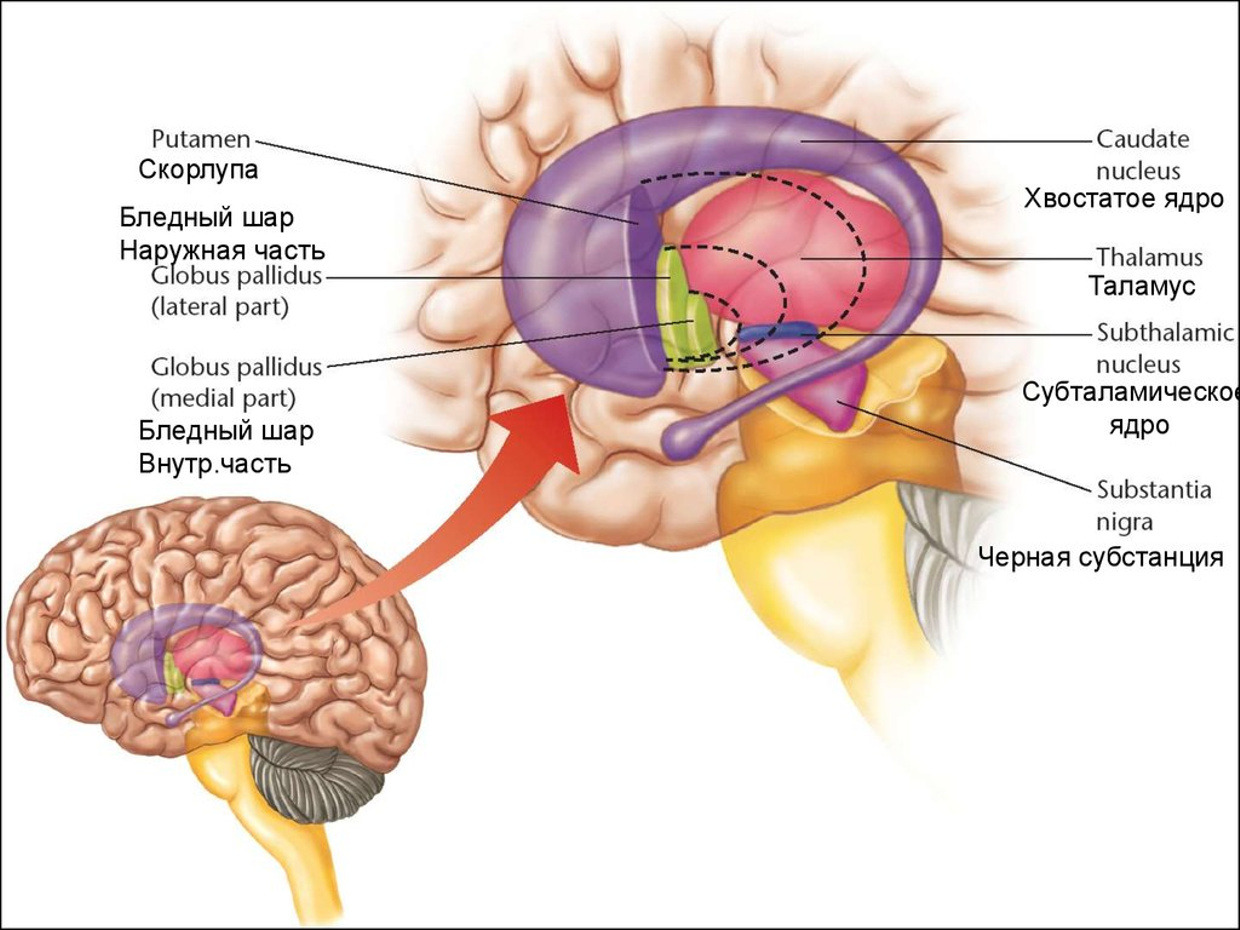
Fig. 9 . Tail core.
The caudate nucleus functions as a part of the “gate” into the basal ganglia, it is associated with the frontal cortex and therefore is involved in high-order cognitive processes. The increased activity of the cortex excites its cells (and the cells of the shell), which, in turn, remove inhibition from the thalamus [23, p. 514].
For our narration, it is important that the tail core contributes to the launch of the correct patterns of actions and the selection of appropriate subgoals based on the assessment of performance (i.e., participates in planning), because Both processes are fundamental to successful, targeted action [24]. Thus, the caudate nucleus can be called the " feedback processor " [31, p. 58]
The ability to perform directed actions is something that often suffers from mental illness.
The caudate nucleus plays an important role in the processes of learning, speech, and the transmission of information about disturbing events between the thalamus and the orbitofrontal cortex.
The increased volume of the caudate nucleus (in comparison with the norm) correlates with impaired spatial working memory [25].
Dysfunction of the caudate nucleus is associated with such phenomena as Tourette syndrome and obsessive-compulsive disorder [38]. In some cases, it makes sense to reduce its activity (more correctly, to return it under the control of the big hemispheres).
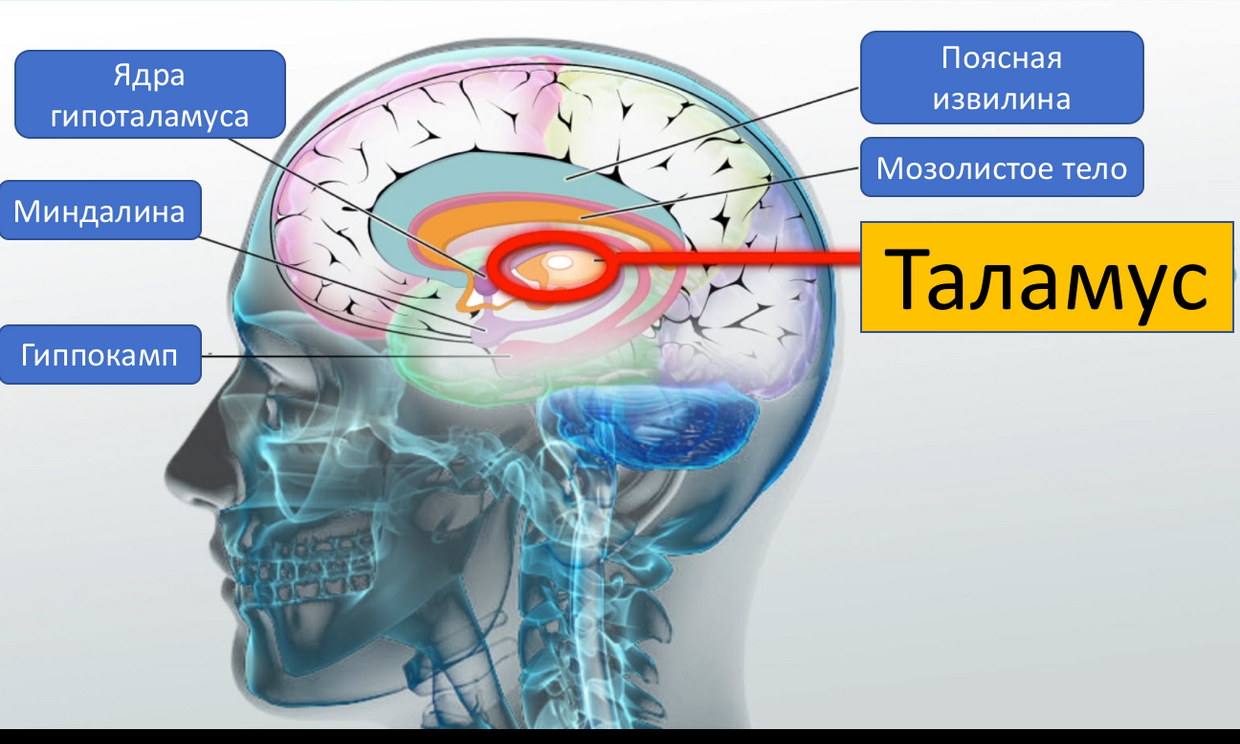
The thalamus (part of the diencephalon) is the most important “neural hub”, where almost all sensory signals (except the sense of smell) are switched, going to the cortex [19, p. 85]
. 10 . Thalamus
The intended function is to receive information from sensors, its primary processing, input and storage [19, p. 201], transfer to the cortex. In some cases, the thalamus increases the activity of the cortex, in others it blocks it [19, p. 122].
The fact that olfactory signals bypass the thalamus allows adherents of perfumery and aromatherapy to talk about the importance of their activities (some smells can be influence the emotional sphere).
Studies on monkeys have shown that the thalamus is associated with compulsive behavior and signs of anxiety [26]. It is believed that the behavior aimed at checking and re-checking, as well as continuous cleaning, is “ sewn ” into the thalamus [27].
Together with the temporal lobes, the thalamus inhibits excessive mood swings that occur in response to daily complex stimuli [10, p. 7185].
The thalamus is a central component for integrating memories of perceptual, somatosensory and cognitive processes [42].
In addition, the thalamus plays an important role in modulating the activity of the amygdala (see above).
The hippocampus , like the amygdala , is located inside each of the temporal lobes of the brain [19, p. 211].
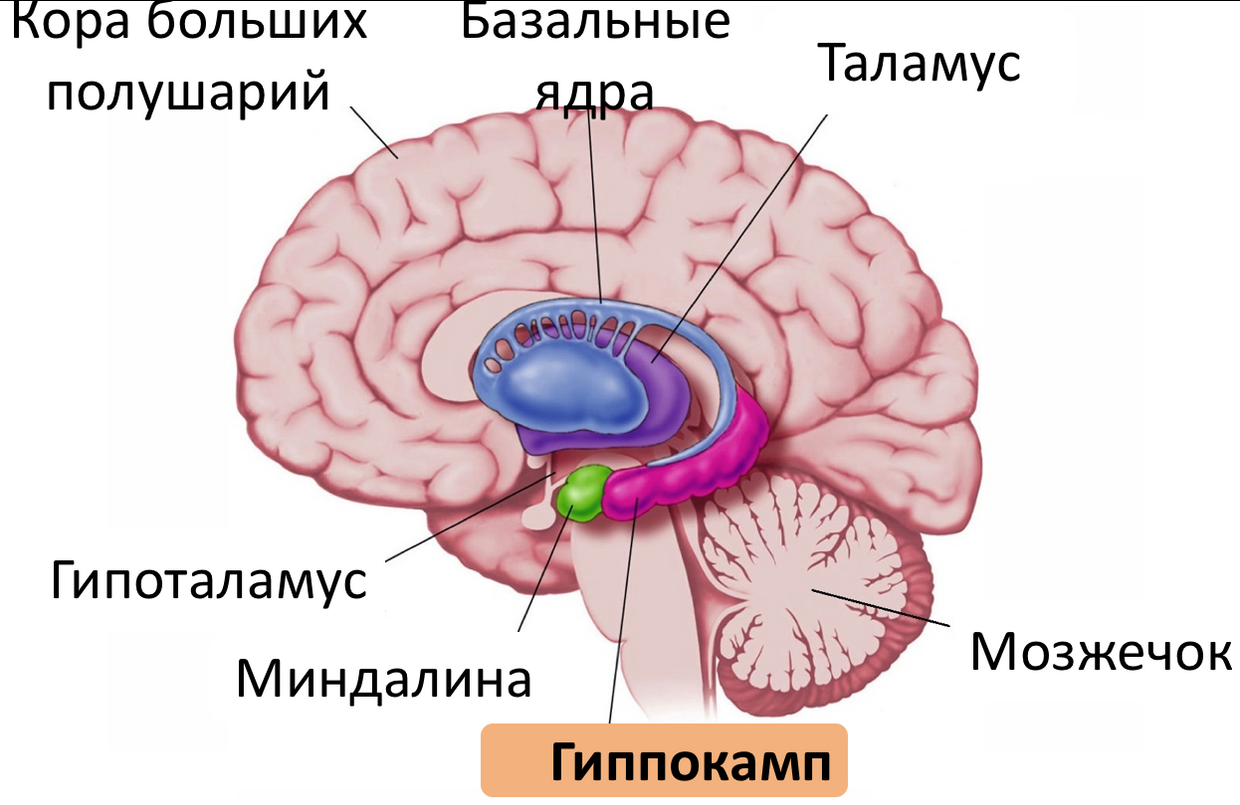
Fig. 11 . Hippocampus.
It plays an important role in the transfer of experimental information to long-term memory, as well as in the extraction of episodic memories, and is related to spatial orientation [19, p. 213].
Studies show that the hippocampus is an important component of the mechanism of consciousness [28]. The hippocampus is one of the few brain structures in which neurogenesis is possible (production of new neurons during life) [19, p. 216]
Together with the amygdala and the limbic cortex, the hippocampus forms the limbic system[19, p. 231]. These structures are closely related to the work of short-term memory (that is, the memory of experience under the control of consciousness) [19, p. 232].
Other studies show that the hippocampus is involved in unconscious memory processes, and that they (conscious and unconscious processes) are related [29] In addition, the hippocampus plays an important role in the processes of spatial imagination, memory formation and access to it [31, p. 65] The
hippocampus (more precisely, its dysfunction) plays an important role in the pathogenesis of such mental diseases as schizophrenia, autism, depression [10, p. 227].
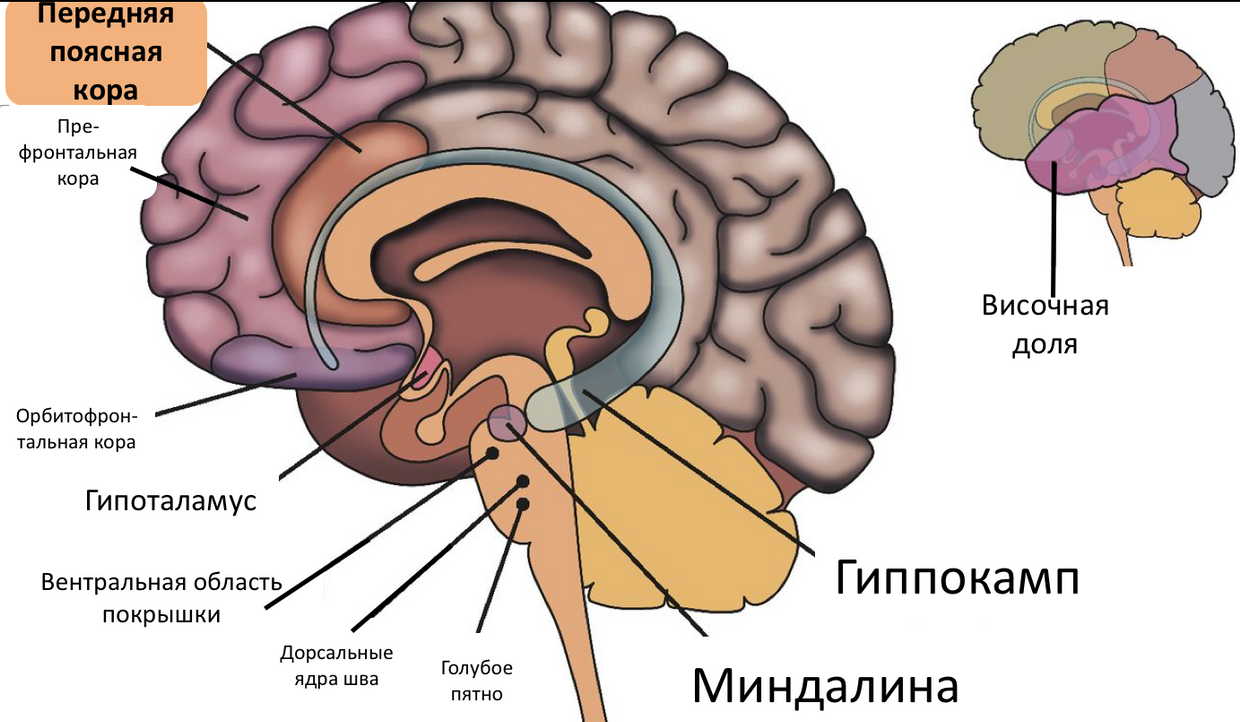
Fig. 12 . Anterior cingulate cortex.
The anterior cingulate cortex performs various functions, of which the most interesting for us are [10, p. 7183]: the conscious regulation of emotions through the re-examination of negative emotions, the suppression of excessive arousal and the suppression of the amygdala.
Those. when we understand that we are “ pounding ” in our fears, and we can consciously reject them, we must say thanks to our anterior cingulate cortex.

Fig. 13 . Prefrontal cortex.
The prefrontal areas of the cortex perform an important control function in the brain. These structures are necessary for arbitrary control. In addition, they participate in emotions and restrain involuntary impulsive reactions [19, p. 93]. The prefrontal cortex is involved in the decision-making process related to moral issues [31, p. 7],
human-conscious feelings arise when the signals of the limbic system reach the areas of the prefrontal cortex that support consciousness [31, p. 39].
The prefrontal cortex is the substrate for the main functions of the ego.[10, p. 7184], together with the amygdala, it controls an essential part of a person’s emotional life and provides adaptability. Disruption of this ligament can cause very acute emotional pain and darken human prudence.
Dorsomedial prefrontal cortex plays a central role in the implementation of downward cognitive modulation (ie, a person’s ability to analyze their feelings, evaluate their “ adequacy ” and, if necessary, suppress them) of fear and other emotions, perception of their emotional reactions and other people's emotional responses - the basis of mentalization and empathy . It is also the physiological basis for object relations [10, p. 7184].
While her activity is lowered, psychotherapy is not particularly effective [10, p. 7184] It is interesting that psychoanalysts, even in those times when visualization technologies were not invented, said that for a successful therapy a patient needs time to “strengthen the ego” (later it turned out that they meant increased activity of the dorsomedial prefrontal cortex).
This was achieved by creating a trusting, supportive relationship, validation, etc. Proper nutrition, rest and moderate exercise were also considered (and are considered) beneficial. Now for these purposes apply incl. antidepressants.
The signals of the prefrontal cortex can “block” pain, and this can be both a conscious and an unconscious process [31, p. 109]
Dorsolateral (not to be confused with dorsomedial, one lateral, the other - medial in spatial terms) prefrontal cortex is a key component of the infrastructure that provides executive functions of the psyche [10, p. 7184]: it relates to the processes of attention, concentration, effort control, operational memory and emotional memory.
The interaction between the amygdala and the prefrontal cortex is crucial for regulating the emotional response to environmental stimuli. [32, p. 6] It is believed that the medial prefrontal cortex regulates and controls the response of the amygdala to its stimuli [20, p. 115]
Technically, it is part of the prefrontal cortex .
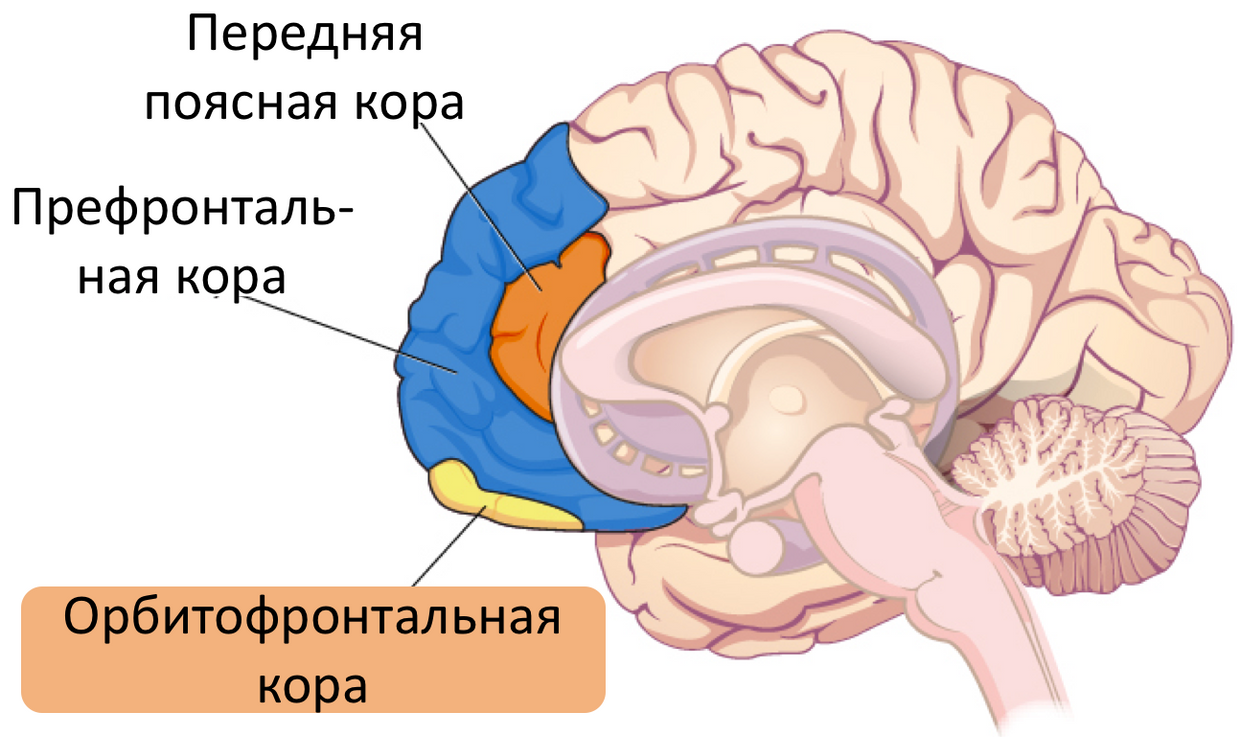
Fig. 14 . Orbitofrontal cortex.
The orbitofrontal cortex inhibits (or strengthens, depending on its condition) impulsive activity in each specific situation in response to the impact of certain kinds of stimuli ( sexual stimulation, risk, excitement ), and is also responsible for the manifestation of pronounced personality characteristics [10, p. 7186]
studies using imaging showed that the euphoria associated with the use of certain substances that correlates with an increase in metabolic activity in the orbitofrontal cortex and reticular formation, while as disf Oriya caused by abstinence, a decrease in activity in these zones [10, p. 7186].
This part of the brain is directly related to decision making [39]. According to the findings of neurobiologist Antonio Damasio [40], in the decision-making process people involve not only the cognitive, but also the emotional sphere: when faced with too complex (contradictory, in conditions of lack of data) choice, a person overloads his makeup, and she stops cope.
This is where the emotional sphere connects, just to make at least some decision, and the orbitofrontal cortex serves as a “ hub ” connecting the cognitive and emotional spheres.
It has been shown [35] that in patients with OCD, the volume of the orbitofrontal cortex of the left hemisphere is less than in healthy people.
Now we will take a very brief look at exactly how the considered (and some other) components of the brain are related to mental illness and mental problems of healthy people. We will not consider here the whole nosology of mental illness (this is the topic of a separate large article), but briefly go over the most famous of them.
When depression reduced activity dorsolateral prefrontal cortex, thereby experiencing experience alone, social isolation and establishment of low productivity standards [10, p. 7185]
Depression is associated with a reduction in the interaction between mandelic and dorsal anterior cingulate cortex [32, p. 6]
Studies using imaging techniques have shown that the subgenual anterior cingulate cortex is excessively active in depression, and some treatments, such as antidepressants, electroconvulsive therapy and transkarnical magnetic stimulation leads to a decrease in activity in this area [10, p. 182].
Some evidence suggests that during depression, the volume of the hippocampus decreases [50].
So far, it has not been possible to establish specific and unambiguous connections between brain areas and schizophrenia, but at the moment this pathology is associated with changes in the hippocampus, entorhinal cortex , multimodal associative cortex, limbic system, tonsil, cingulate cortex, thalamus and medial temporal lobe [10 p. 239].
Currently, there are two main ways to explain the pathophysiology of OCD: through the cortico-thalamic-cortical pathway and through the connection of the limbic system and the cortex [30].
Insel cites data [36] based on an analysis of studies using visualization, according to which OCD symptoms are explained by pathology in three regions of the brain: the orbitofrontal cortex, the cingulate cortex and (to a lesser extent) the caudate nucleus: excessive activity in the head portion of the caudate nucleus suppresses (inhibits ) transfer to the fibers of the white ball, which usually quenches the activity of the thalamus.
As a result, the thalamus increases the activity of the orbitofrontal cortex, which, through the cingulate cortex, closes at the head of the caudate nucleus, forming a cycle of positive feedback.
In contrast to the above nosological units, the early non-maladaptive schemes themselves are not a mental illness: there is no such diagnosis.
However, it makes sense to include them in this article, since they are very widespread in healthy people and significantly hinder them.
What is the early maladaptive scheme (hereinafter - just a “ scheme ”)? A scheme is such a psychic construction that includes memories, thoughts, emotions, and body sensations. And they do not simply enter, but in a cunning manner are interconnected and interdependent [48, p. 41].
The scheme is formed somewhere in the early history of the life of an individual (usually in childhood, but maybe later) as a reaction to some events or phenomena of relationships with people significant for this person (the very "papa beat, mom didn’t like "). The
amygdala keeps unconscious information about trauma / negative emotional experience.
When a person encounters stimuli resembling events that led to the formation of a pattern, the amygdala triggers an unconscious process of activating those very emotions and physical sensations. faster than a person manages to understand anything.
When the circuit is activated, the person covers the wave of emotions and bodily sensations. It is not always aware of the connection with the lived experience of the original trauma.
Osozna aemye memories of trauma are stored in the hippocampus [48, p. 41] and the higher regions of the cortex. In fact, the emotional and cognitive aspects of traumatic experiences are stored in different parts of the brain.
Example of the scheme: a boy as a child climbed into his father's toolbox, his father brutally beat him. Many years have passed, the boy has grown and will present a certain project to customers. Everything is good with him - he copes with anxiety, he is thoroughly prepared, but here one of the listeners asks him a question ...
And the amygdala is activated (for example, from a tone or some characteristic word), launching the scheme. The speaker is unsettling this question, he begins to worry, forget details, feel incompetent, sweating, trembling, etc.
The task that is usually put in working with schemes is to strengthen the control of the prefrontal cortex over the amygdala.
Now that we have at least some understanding of how conversational therapy should affect the brain, and how this very brain works, it's time to talk about the results of research, the purpose of which was to evaluate the effect of psychotherapy on the morphological and biochemical characteristics of the brain.
In a meta-analysis [32], a significant relationship was found between the effect of therapy on the rostral anterior cingulate cortex and the precentral sulcus (increased activity), which more or less coincides with the initial assumptions.
The ventral rostral prefrontal cortex has extensive connections with brain regions responsible for processing emotions, in particular, with the amygdala. In addition, she participates in the decision-making process and the reward system.
In healthy people, the regulation of emotions is associated with the suppression of the activity of the tonsil by the rostral and dorsal cingulate cortex and some regions of the anterior cingulate cortex. Those. “Fear coming from the depths” in response to a stimulus at some point is intercepted, analyzed and “canceled.” Jugging on negative thoughts that is
characteristic of depression can be explained by a decrease in the level of connection between the cortical and amygdala. “ I am a loser ,” “ everything will be bad, ” etc. The increased activity of the rostral cingulate as a result of the use of psychotherapy may reflect improvements in emotional regulation and may be a possible basis for a cognitive reappraisal mechanism .
A cognitive revaluation is essentially one of the cornerstones of KPT. It lies in the fact that automatically arising negative thoughts to catch and analyze, and then replaced by more adequate (not containing cognitive distortion).
The increased activity of the anterior cingulate cortex is manifested after a course of CPT, and, after a course of long-term psychodynamic therapy, this activity decreases [32, p. 18].
However, the authors do not give any interpretations about this, and we will not invent a gag. Perhaps the point here is that in some studies the whole cortex is considered entirely, and in others the subgenual part of it (reduction in the activity of which correlates with a decrease in the feeling of guilt and oppression of repressed emotions).
Long-term verbal therapy leads to a decrease in activity in the left precentral gyrus , which is usually associated with motor functions, but may be involved in the processes of cognitive functioning.
A systematic study showed a weakening of the activity of the amygdala as a result of the use of CPT and psychodynamic therapy [32, p. 19]. And since the amygdala is the “center of fear” (again, a very, very figurative analogy), a decrease in its activity should lead to a decrease in the severity of depressive and anxious symptoms.
In another systematic meta-study [37], the authors concluded that anomalies in the hippocampus, amygdala, lower frontal gyrus, hookas well as in areas actively involved in managing emotions (dorsolateral prefrontal cortex and anterior cingulate cortex) are predictors of successful psychotherapeutic treatment of anxiety disorders.
Or, if one could fantasize a little, then with some stretch one can say that with successful treatment of anxiety disorders, changes in these areas will be observed.
In a study of the effects of psychotherapy in depression, it was shown [41] that conversational therapy leads to the normalization of the connections between the limbic system and the cortex, especially in the anterior cingulate cortex. In the same study, the use of islet fraction activity was suggested.as a biomarker that will help the doctor determine which treatment method is best suited in this particular case - psycho-or pharmacotherapy.
In a meta-study [42] of therapy by the method of desensitization and processing by the movement of the eyes (not quite colloquial therapy, the essence of which is to recall traumatic memories and move your eyes to and fro, no matter how funny it may sound), a change in the pattern of interaction between hemispheres.
It also presented data indicating an increase in the volume of the hippocampus, an increase in the activity of the anterior cingulate cortex, and the left frontal lobe. These and other data suggest that this therapy leads to increased control of the prefrontal cortex over the too active limbic system.
A study of the effects of long-term psychodynamic psychotherapy has shown that this treatment reduces the activity of the amygdala / hippocampus, subgenual cingulate cortex and medial prefrontal cortex [44]. These changes correlated with a decrease in the symptoms of depression.
Well, research quite convincingly shows us that the brain changes under the influence of verbal therapy. But how exactly does he do it?
The answer lies in its such property as neuroplasticity. More precisely, not so: there is no direct evidence that psychotherapy increases brain neuroplasticity, but the common place is the idea that this very neuroplasticity is somehow involved in the process of psychotherapy [49].
As applied to the nervous system, neuroplasticity is the ability of nerve elements and regulatory molecules to adaptive reorganization under the influence of endogenous and exogenous influences [46, 79].
Neuroplasticity is observed at different levels [47] - at the level of the brain as a whole, at the level of its individual components, at the level of neurons, and even at the subcellular level.
The fundamental component of neuroplasticity is the plasticity of synaptic connections (ie, connections between neurons), which constantly disappear and reappear, and the balance of these opposite processes depends primarily on the activity of neurons [47].
The dependence of synaptic plasticity on activity is one of the central points of the concept of neuroplasticity, as well as theories of learning and memory, based on the experience of changes in the structure and function of synapses.
Long-term plasticity is realized as a result of changes in the expression of genes triggered by signaling cascades, which, in turn, are modulated by various signaling molecules with changes in neural activity.
A detailed examination of the molecular mechanisms of neuroplasticity is clearly beyond the scope of this article, so we will focus on the fact that the ability of the brain to change under the influence of external influences is proven. And it allows you to implement all those changes, which were discussed above.
Here we will talk about some additional hypotheses about exactly how therapy can affect the brain:
1. Perhaps psychotherapy affects the levels of neurotransmitters, in particular, serotonin . A review [49] showed that patients suffering from bipolar affective disorder and depression and who had lower serotonin levels (compared to the control group) in the prefrontal cortex and thalamus before the start of treatment showed an increase in serotonin levels in these areas after a year’s course of psychodynamic therapy. True, the study on the basis of which this conclusion was made has a less than ideal design (small sample, lack of successful reproduction).
2. It is possibletherapy affects the thyroid axis . The same review [49] refers to a study that showed that depressed patients who responded successfully to CPT achieved a reduction in T4 (thyroid hormone) levels, while patients who did not respond to therapy had it boost
3. Perhaps psychotherapy stimulates processes related to the neuroplasticity of the brain . As mentioned above, there is no clear evidence that psychotherapy leads to an increase in brain neuroplasticity, but there is evidence from animals, according to which training leads to it.
It is believed [49] that learning occurs through psychotherapy, which leads to an increase in the synaptic potentials of the neurons of the perforator path connecting the entorhinal cortex with the dentate gyrus of the hippocampal formation.
The same increase was demonstrated in animal models: rats that had undergone spatial orientation training had a greater density of dendritic spines compared with the two control groups.
Since the length of the dendrites, as well as the structure of their branching, remained unchanged, conclusions were made about the formation of new synapses.
Of course, directly transferring data from animal models to humans, and even taking into account different activities (direct learning in one case and psychotherapy in another) is not entirely correct, but some authors [49] consider it possible to use these data as an argument in the benefit of the hypothesis that psychotherapy alters the brain at the physical level.
Talking therapy can lead to significant changes in the brain. Naturally, not only is she - various mental exercises, meditation, and life experience in general, also use neuroplasticity to form the corresponding connectome.
However, studies show that during conversational therapy, these changes reach a higher level than in its absence.
The question of whether it is possible to use neuroplasticity for self-therapy, I will leave unanswered for the time being: the article turned out to be too long.
And here is the promised video version for those who preferto listen to all garbage in the background on accelerated playback to watch, not read:
Sorry for the quality of the broadcast, it's terrible, I know.
previous articles were mainly devoted to questions of pharmacology, but this is not really my topic, I am still a clinical psychologist (more recently), so today we will talk about conversational therapy in all its manifestations. tl; dr : in a long and tedious article addresses the issue of the effectiveness of psychotherapy ( yes, effective, within its limits of applicability, of course ), and also provides reflections on how this efficiency is achieved ( through the implementation of morphological and metabolic changes due to brain neuroplasticity ) .
At the end of the bonus for fans of video format (if there are any): record the presentation on the topic of this article: if you are lazy to read, you can see.
What is psychotherapy
According to the definition adopted by the American Psychological Association, psychotherapy
“This is a deliberate and informed use of clinical [psychological] methods and interpersonal relationships, aimed at achieving changes in behavior, thinking, emotional responses, and other personal characteristics in a direction that participants consider desirable” [1].
For the purposes of this article, we will not draw a rigid distinction between psychotherapy proper and psychological counseling, which is defined as
“Professional assistance to a person or a group of people in finding ways to resolve or solving a certain difficult or problematic psychological situation” [2, p.3]Despite the fact that in the Russian tradition to emphasize the differences between them is considered good form, some authors recognize the similarity of these practices and group them into the category of " psychological, more precisely, clinical and psychological interventions " [2, p. 3]
In general, you already guessed , it will be about all forms of interaction between the specialist and the client (doctor and patient) when using word effects: from classical psychoanalysis to modern behavioral and cognitive-behavioral approaches. Or, to put it more simply, about " talking with a psychologist / psychotherapist ."
Why do you need it when there are pills
Indeed, we live in the 21st century, more and more sophisticated psychiatric drugs are offered to the market each year , intended to treat slightly less than all known mental disorders [3], and the relevance of psychological / psychotherapeutic influences is questioned by many.
However, there are reasons for using conversational (non-drug) methods.
First , they are in some cases just as effective as drug treatment: in the case of depression [4,5], panic disorder , social phobia [5] and even psychosis [6].
Secondly , in some cases they are more effective than drugs: in the treatment of OCD[5], some types of depression [8].
Thirdly , often the joint use of drugs and psychotherapeutic methods is more effective than only drug treatment [6,7,45].
Fourth , in some cases they have fewer side effects and are more easily tolerated [6].

Fig. 2 . Treatment with CPT and pharmacotherapy has led to a significant decrease in the activity of the tonsil in situations of anxiety. Source: [45]
Of course, I would not like the reader to get the wrong impression of psychotherapy as a panacea: in some cases, some methods of conversational influence are not only not useful, but also harmful (for example, “unstructured” types of psychotherapy when working with patients sufferingborderline personality disorder ) [9]. In the end, the measure of therapeutic effects determines the doctor in each case .
The attentive reader may note that this section is about psychotherapy, but not about psychological counseling.
Indeed, the latter has been studied much worse - both because of insufficiently developed research methodology ( how to evaluate the success of counseling during a divorce - not by the number of preserved marriages? ), And because of the much smaller prevalence of the principles of "evidence".
What kind of psychotherapy is effective?
There are a great many types of psychotherapy [10]: cognitive , behavioral , cognitive-behavioral , rational-emotional-behavioral , narrative , psychodynamic , psychedelic , interpersonal , gestalt therapy , logotherapy , sensitization and processing by eye movement , etc.
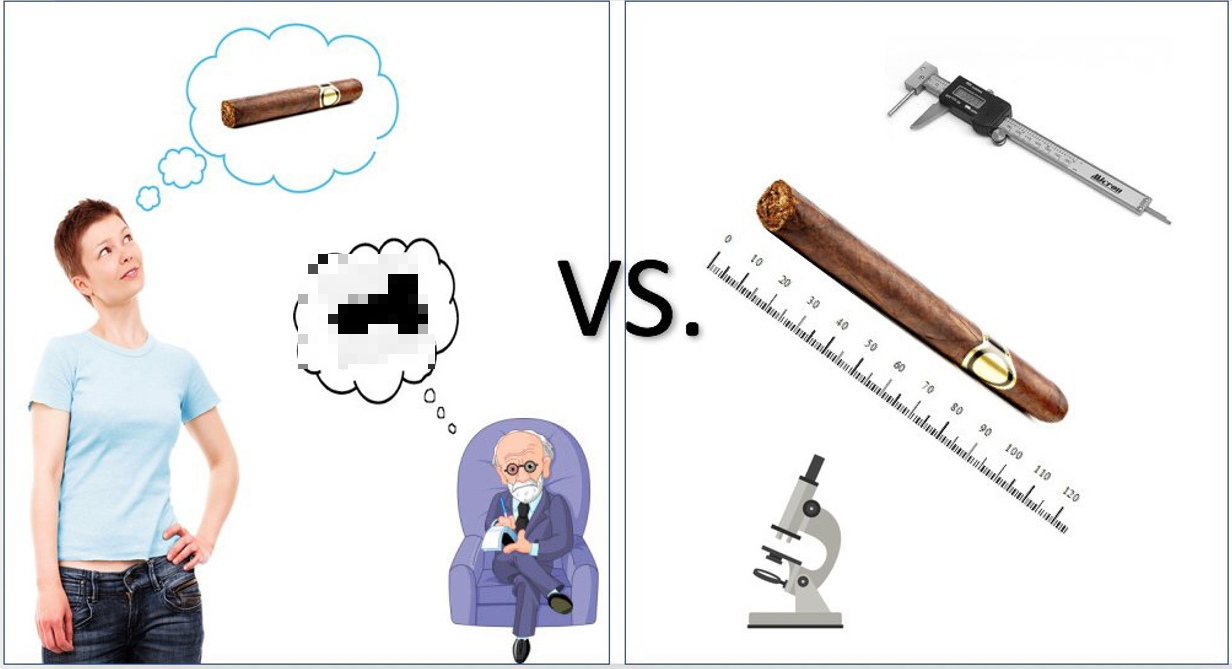
Fig. 3 . From the Freudian associations [first level] to modern methods of therapy based on the principles of evidence.
And each school claims to be considered effective. And in some areas there is a completely imputed evidence base. At the same time, in most cases, explanations of this very efficiency are conducted through constructions adopted within the framework of this approach and are not quoted anywhere outside this framework.
So, for example, logotherapists believe that they achieve positive results by helping the patient find the meaning of life [11], supporters of the cognitive approach - by working with negative automatic thoughts [12], representatives of the psychodynamic direction - by working with the transference, drive and object relations [13], supporters of psychedelicthe approach is due to the work with perinatal matrices and systems of condensed experience [14] and etc.
At the same time, the majority of such explanations lose all convincingness as soon as they fall outside the context of the theory that generated them. So, for example, the cognitive postulate that thoughts affect emotions [12] is completely unacceptable within the psychodynamic school, where a completely opposite view is used.
Contrary to the opinion prevailing in the domestic environment, proven clinical efficacy ( to the extent consistent with the principles of evidence-based medicine , which is generally possible for psychotherapy) has not only cognitive-behavioral, but also, for example, psychodynamic therapy [15,16,17]. Those. different therapies based on completely different sets of axioms show comparable effectiveness.
Modern authors have noted [10, p. 7190] that all approaches to psychotherapy have a common base that ensures effectiveness:
“The relationship between therapist and client, in which different roles carry a different set of expectations and responsibilities; impartial and unconditional acceptance of the client by the therapist; a union whose goal is to work on common goals. ”However, these categories are too “ hypothetical ” and “ psychological ” (and therefore poorly formalized ) to be satisfied with them as an explanation of the effectiveness of “therapeutic conversations”.
One of the most interesting attempts to isolate and describe quantitatively the universal basis of successful therapy is the study of German authors [18], in which it was found that the predictor of the success of therapy is the difference in emotions that appear on the therapist’s face and those expressed by the client during the narration.
In other words, if during the first session a sad-faced client speaks about his pain (expressing " negative emotion"), and the therapist listens to him, demonstrating interest and satisfaction (" positive emotion "), the therapy is likely to be successful. If both express emotions of the same direction (" positive "/" negative "), then no.
The authors formally formalized the procedure testing, making a very limited “glossary” of emotions and selecting only those expressions of people that exactly matched him. As for determining the success of therapy (also not an easy task), we used therapist’s and patient’s estimates and objective indicators with symptom reduction.
Their conclusions are quite different from the predictions and explanations that psychotherapists themselves give - they talk about anything: about motivational readiness, about the radical of the client’s personality, about the level of organization of that person, about the deep patterns - but not about those emotions they express with their faces.
Such studies make us somewhat skeptical about the supposed mechanisms for realizing beneficial changes that psychotherapists / psychologists are talking about, and are pushing to find some more convincing ways to explain the existence of these very changes.
Therapy and brain changes
Some time ago, there was no way to objectively evaluate the effect of therapy on the brain, so psychotherapists made the most courageous (and often incorrect) assumptions about the presence and nature of such an effect.
Naturally, this situation could not last forever, and as soon as researchers had available methods for imaging the brain ( PET , MRI , fMRI , SPECT ), studies were published that aimed to determine the extent of the impact (or lack thereof) of conversational therapy on the physiological substrate of the brain .
Identifying this influence would solve several important problems - from the proof that conversational therapy works in general, to understand how it works, whether there is a difference between different types of therapy, etc.
Below is my attempt to systematize the data on the visualization of changes caused in the brain by speaking therapy.
It does not claim to be universal, but when it was created, I tried to include more or less sane studies and recheck the conclusions of the authors.
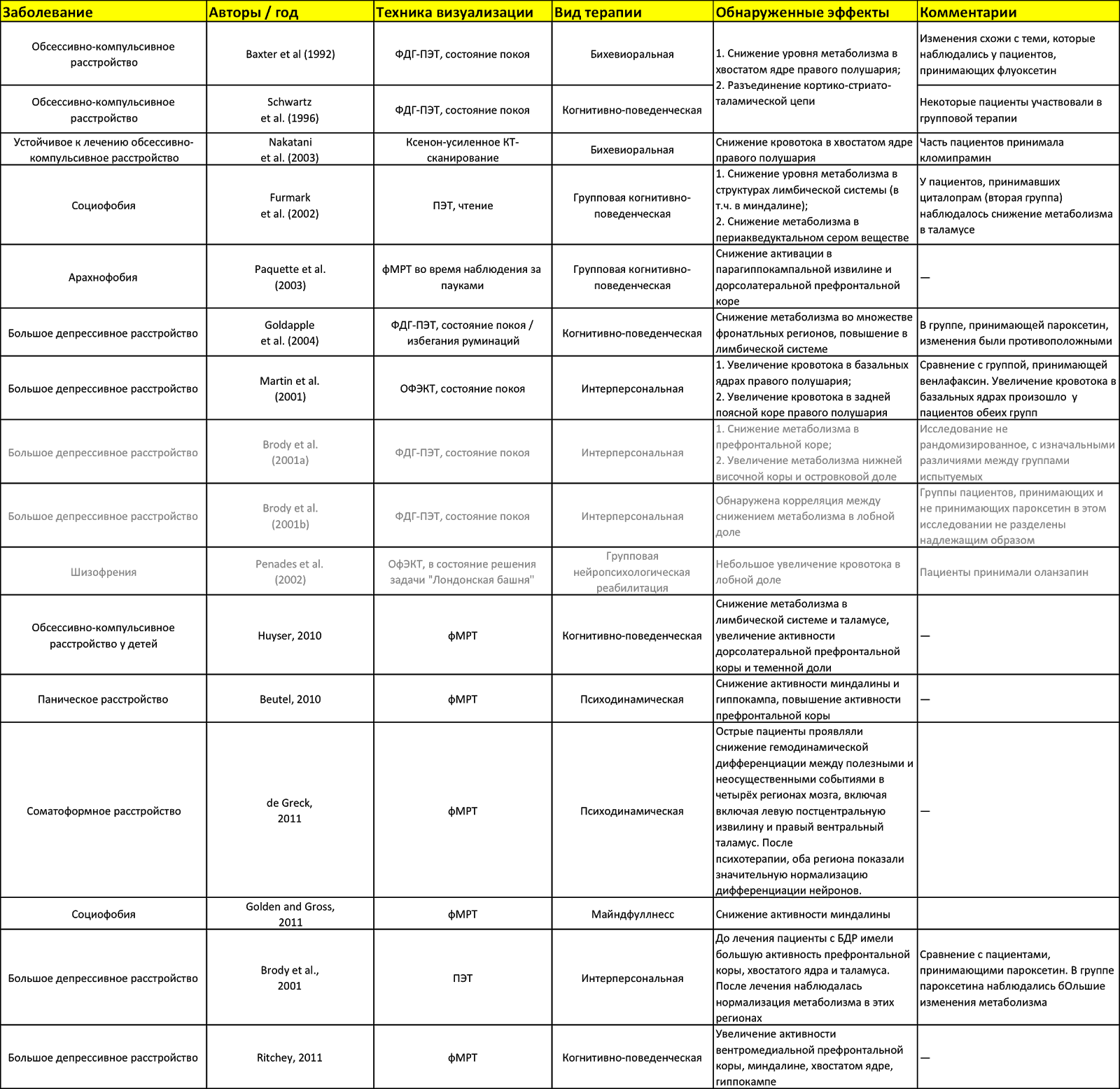
Fig. 4 . The effect of speaking therapy on the brain. Sources: [10, 32, 33, 34]. The table is available in Google Docs .
What do we see in this table? The first thing that catches your eye is the fact that the same areas of the brain (for example, the caudate nucleus or the amygdala) are affected by completely different types of therapy.
The second- this is what in some studies the activity of certain areas increases (for example, the amygdala in the Ritchey study), and in others, with the same therapy, it decreases (the limbic system, including the amygdala, in the study of Goldapple).
The third is that some studies are marked in gray. These are those whose design caused me the greatest doubts. But since today there are not so many such studies at all, I included them here.
What is the result? Visible some inconsistency data. It is caused by the fact that, firstly, the brain is a complex and controversial thing (I seem to have already spoken about this), and, secondly, by the fact that the research did not have a completely identical methodology.
What is the value of this table, if you can not directly compare different methods of PT? It is possible to make sure that conversational therapy “ does something with the brain there ”, and also that you can try to build some cautious conjectures on how this conversational therapy works.
But first, let's try to still highlight some patterns in these changes. To do this, we will not peer into the table for a long time, but use the data from the finished meta-analyzes.
Assumptions about the effect of conversational therapy
It is assumed that with depression, CPT enhances cortical control on the part of the prefrontal cortex (especially its dorsolateral part), which inhibits (inhibits) impulses of subcortical structures [32, p. 6].
What this means: impulses that rise “ from the depths of the unconscious ” (this is just a beautiful metaphor) begin to be better controlled by structures that are more related to rational thinking.
If we recall how KPT works - namely, it is trying to replace “ automatic thoughts filled with cognitive distortions with more sober and rationalistic assessments of the situation ”, then we can trace some logic in this whole thing.
Therapy aimed at activating behavior presumably leads to the activation of the striatum and the activation of the reward system, including regions of the dorsolateral prefrontal and orbitofrontal cortex [32, p. 6]
What does this mean: again, the activation of “ more conscious structures ” as well as responsible for the behavior (as a set of motor, ie physical actions).
It is logical: we activated the behavior, activated the structures that are responsible for it. Since this therapy is essentially behaviorism, it is not surprising that the structures responsible are inclusive, incl. for reflexes and analysis of encouragement / punishment.
Overcoming repressed emotions and weakening unconscious guilt, which are important componentspsychodynamic therapy is presumably associated with a decrease in the activity of the subgenual anterior cingulate cortex [32, p. 6].
Everything is quite interesting here, since this very subgenual PPK is involved, including in overcoming feelings of fear (here you can draw far-reaching conclusions that, perhaps, psychodynamics are right, and the repressed guilt is therefore supplanted, because the psyche is “afraid” to accept it, but this will lead us away to speculations).
It should be noted that these assumptions appeared not from scratch, but on the basis of other studies (there are links in [32] on the corresponding pages).
A little about the brain
Before discussing the results of research on the effect of colloquial therapy on the brain, you need to at least talk a little about how it works and consider some of its components that are directly related to the subject of the article in order to understand what the researchers have been doing there.
The main thing that can be said about the brain: it is complex . There are only so many ways to consider it that an unprepared person has a head in a circle — all these columns , departments , cortical maps , functional blocks , Brodmann fields , etc.
Fig. 5 . The progress of psychiatry and neuroscience through the eyes of the inhabitant.
We will not try here to examine the structure of the brain from all possible points of view, but only fragmentarily describe those parts of it that are relevant to the subject of this article.
It should be noted that the brain is a distributed system with a high degree of parallelism [21, p. 132], therefore, to say that one or another part of it performs a specific limited function would not be completely wrong. That is why all phrases like (“the amygdala is responsible for fear reactions ” should be taken as more or less successful analogies / metaphors, nothing more).
However, to some extent its components are specialized, and we will try to consider this specialization in the context we are interested in.
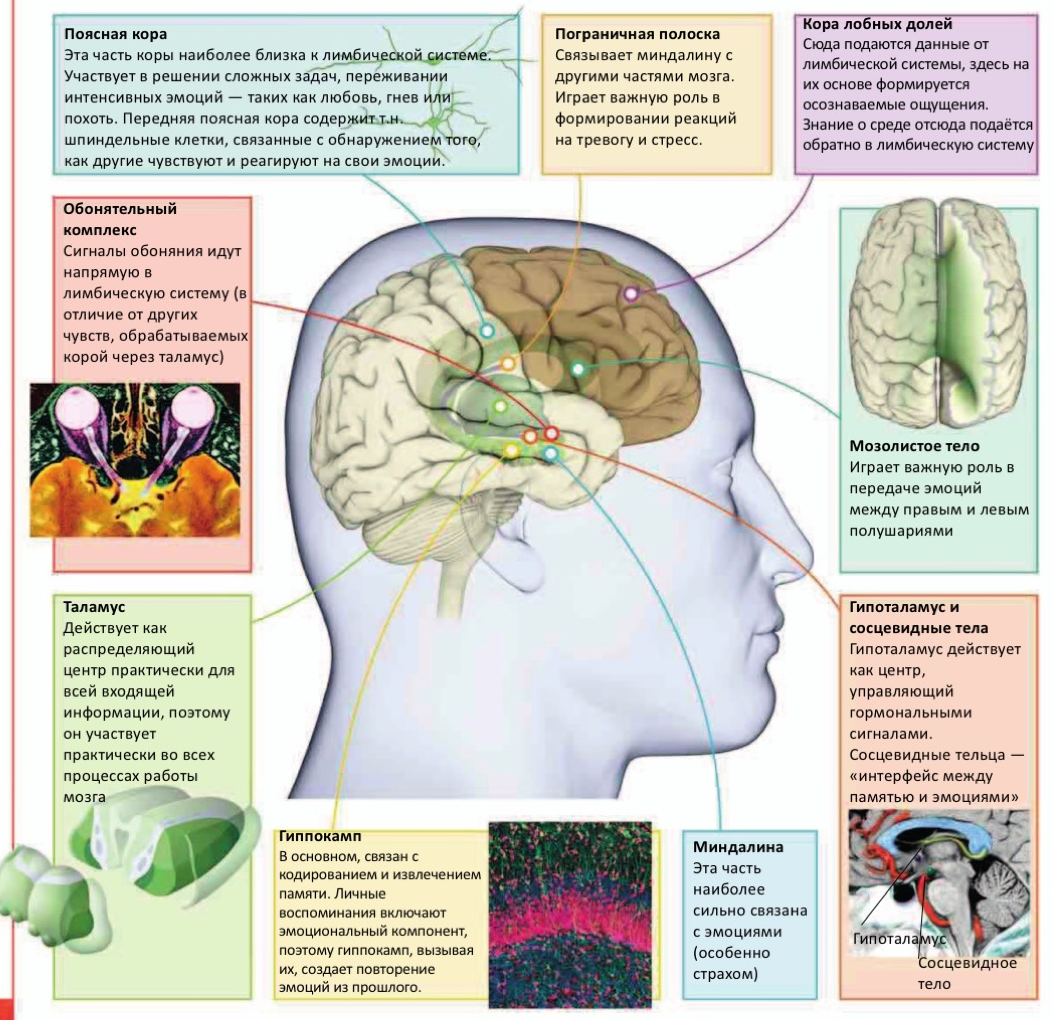
Fig. 6. Some components of the brain relevant to the subject of this article [31, p. 126].
Amygdala
The amygdala, it is also the "almond-shaped body." Located in the temporal lobe (median temporal lobe) [19, p. 232]. Since we have two hemispheres and two temporal lobes, respectively, are also two, then the amygdala is “divided into two pieces”. [19, p. 211]. This, by the way, applies not only to the amygdala.
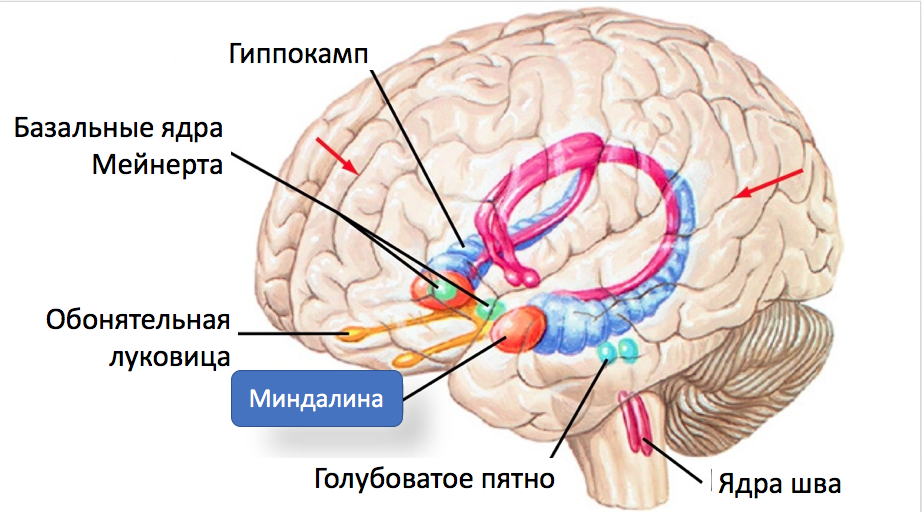
Fig. 7 . Tonsil and some of her connections.
Connecting with the prefrontal and temporal cortex , as well as with the spindle-shaped gyrus of the amygdala, plays a significant role in social and emotional cognition [10, p. 240] and is considered the main center for processing emotional information [19, p. 482].
Equally important is the fact that the amygdala is connected to the hippocampus[19, p. 216], which is involved in memorizing information (memory consolidation from short-term to long-term), its processing and retrieval from memory [19, p. 78].
The amygdala is part of the so-called. limbic sistama. It is shown that the structures of the limbic system and the nucleus accumbens participate in the “final calculation of remuneration”, assigning characteristics of pleasure or displeasure to the affective experience, and the warning / arousal system uses the reticular formation , thalamus, amygdala and cortex to assign personal experience and significance to this experience [ 10, p. 7186].
Studies have shown that the amygdala responds to emotional stimuli [19, p. 297] and mediates the conditioned-reflex reaction of fear [19, p. 538].
The dynamic interactions between the amygdala and the medial prefrontal cortex (mPFC) are conceptualized as a system that allows us to automatically respond to biologically significant stimuli, and also to regulate these reactions when the situation requires it [20, p. 113].
The amygdala has two “inputs” through which it receives sensory information. First, data comes from the senses to the thalamus , then they follow one of two independent paths: either directly to the amygdala, or first pass through the prefrontal cortex , and then reach the amygdala through the anterior cingulate cortex.[22, p. 19]:

Pic. 8 . Two modes of activation of the tonsils.
The first path is “ quick and dirty ” - the amygdala receives information that some kind of tin is created in the outside world, and does not go into details of what exactly this stimulus was: it starts to act, without taking time to figure out in a situation.
The second way is slower, but involves some analysis of incoming information. Data is processed in the prefrontal cortex.which integrates sensory information from the senses with information about the context of this stimulus received from the hippocampus, compares it with the experience stored in long-term memory, analyzes the previous similar situations and decides how real the danger is. She sends this decision to the amygdala, which, in the case of a positive response, triggers the preparation of the organism for the “flight or attack” reaction.
If the cortex " recognized the stimulus as harmless, " the amygdala on the contrary inhibits the stress response [22, p. 19].
For example, if an unprepared person noticed a snake in his path, it is highly likely that his amygdala will be activated by the thalamus without the participation of the cortex. At the same time, if it is a gerpentologist who understands that the snake is not dangerous, then, quite possibly, his reaction will follow the second scenario.
It has been shown [10, p. 7184] that the activity of the amygdala is elevated in depression and post-traumatic disorders . The situation is even worse if an increase in the activity of the amygdala is combined with a decrease in the activity of the prefrontal cortex.
Those. It is beneficial for us to reduce the activity of the amygdala, either directly or indirectly, through increased activity in the prefrontal cortex (see above data on the corresponding changes as a result of psychotherapy).
Tail core
The caudate nucleus (along with the shell-core, which together form the neostriatum ) are part of the basal ganglia , which are connected by afferent (sensory, "incoming") and efferent (motor, "outgoing") connections with the structures of the midbrain - the black substance and subtalamic nucleus .
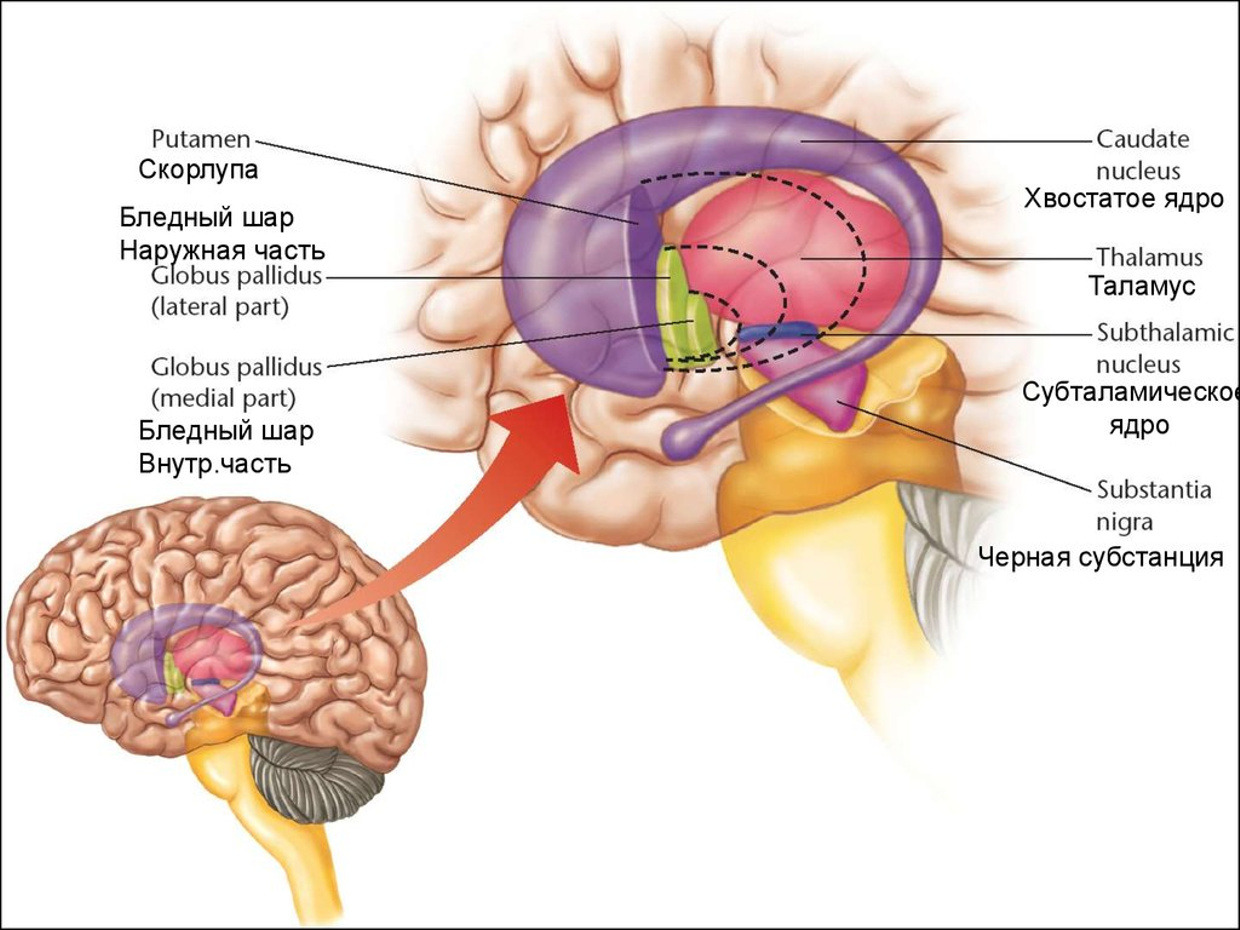
Fig. 9 . Tail core.
The caudate nucleus functions as a part of the “gate” into the basal ganglia, it is associated with the frontal cortex and therefore is involved in high-order cognitive processes. The increased activity of the cortex excites its cells (and the cells of the shell), which, in turn, remove inhibition from the thalamus [23, p. 514].
For our narration, it is important that the tail core contributes to the launch of the correct patterns of actions and the selection of appropriate subgoals based on the assessment of performance (i.e., participates in planning), because Both processes are fundamental to successful, targeted action [24]. Thus, the caudate nucleus can be called the " feedback processor " [31, p. 58]
The ability to perform directed actions is something that often suffers from mental illness.
The caudate nucleus plays an important role in the processes of learning, speech, and the transmission of information about disturbing events between the thalamus and the orbitofrontal cortex.
The increased volume of the caudate nucleus (in comparison with the norm) correlates with impaired spatial working memory [25].
Dysfunction of the caudate nucleus is associated with such phenomena as Tourette syndrome and obsessive-compulsive disorder [38]. In some cases, it makes sense to reduce its activity (more correctly, to return it under the control of the big hemispheres).
Thalamus
The thalamus (part of the diencephalon) is the most important “neural hub”, where almost all sensory signals (except the sense of smell) are switched, going to the cortex [19, p. 85]
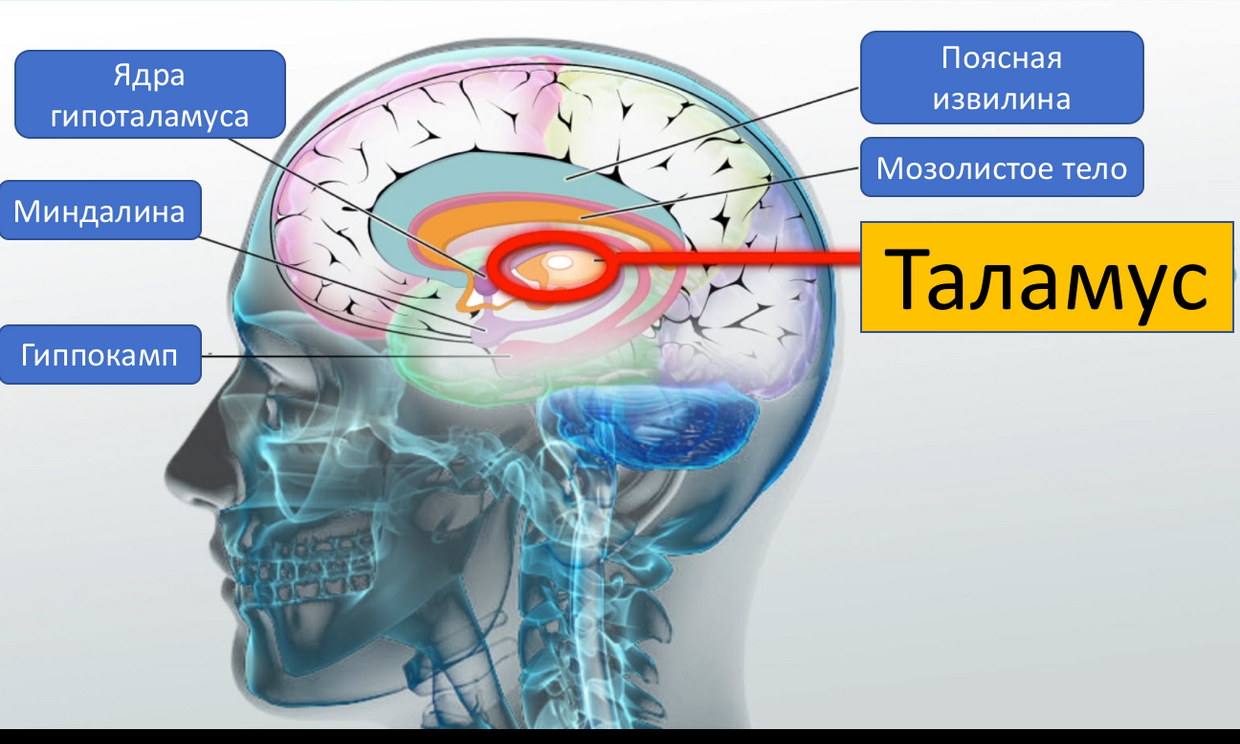
. 10 . Thalamus
The intended function is to receive information from sensors, its primary processing, input and storage [19, p. 201], transfer to the cortex. In some cases, the thalamus increases the activity of the cortex, in others it blocks it [19, p. 122].
The fact that olfactory signals bypass the thalamus allows adherents of perfumery and aromatherapy to talk about the importance of their activities (some smells can be influence the emotional sphere).
Studies on monkeys have shown that the thalamus is associated with compulsive behavior and signs of anxiety [26]. It is believed that the behavior aimed at checking and re-checking, as well as continuous cleaning, is “ sewn ” into the thalamus [27].
Together with the temporal lobes, the thalamus inhibits excessive mood swings that occur in response to daily complex stimuli [10, p. 7185].
The thalamus is a central component for integrating memories of perceptual, somatosensory and cognitive processes [42].
In addition, the thalamus plays an important role in modulating the activity of the amygdala (see above).
Hippocampus
The hippocampus , like the amygdala , is located inside each of the temporal lobes of the brain [19, p. 211].
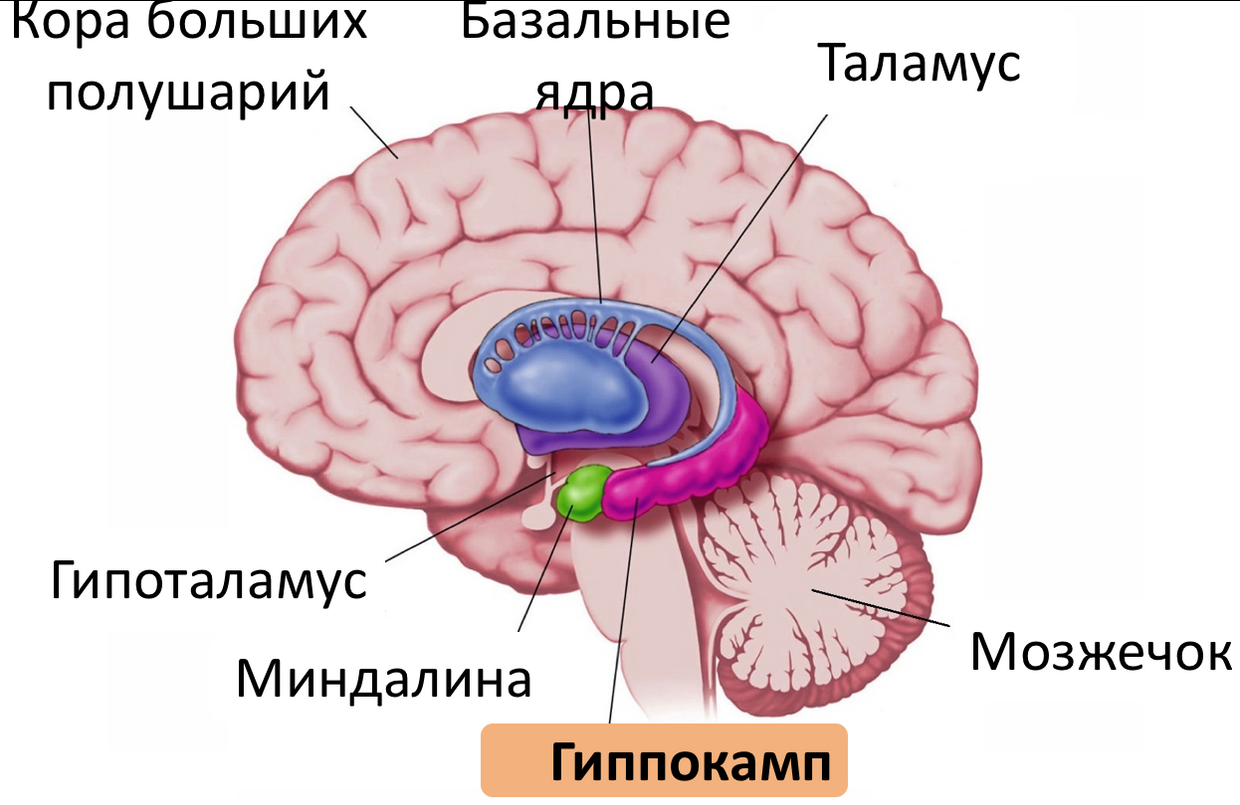
Fig. 11 . Hippocampus.
It plays an important role in the transfer of experimental information to long-term memory, as well as in the extraction of episodic memories, and is related to spatial orientation [19, p. 213].
Studies show that the hippocampus is an important component of the mechanism of consciousness [28]. The hippocampus is one of the few brain structures in which neurogenesis is possible (production of new neurons during life) [19, p. 216]
Together with the amygdala and the limbic cortex, the hippocampus forms the limbic system[19, p. 231]. These structures are closely related to the work of short-term memory (that is, the memory of experience under the control of consciousness) [19, p. 232].
Other studies show that the hippocampus is involved in unconscious memory processes, and that they (conscious and unconscious processes) are related [29] In addition, the hippocampus plays an important role in the processes of spatial imagination, memory formation and access to it [31, p. 65] The
hippocampus (more precisely, its dysfunction) plays an important role in the pathogenesis of such mental diseases as schizophrenia, autism, depression [10, p. 227].
Anterior cingulate cortex
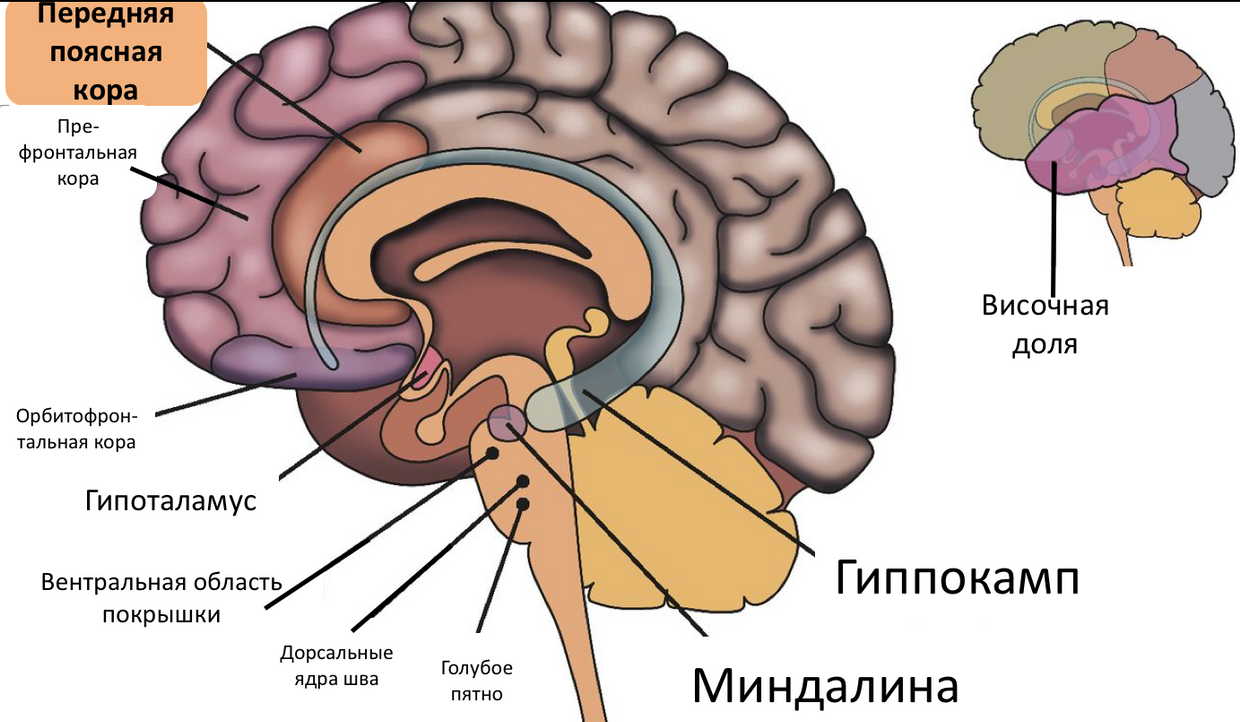
Fig. 12 . Anterior cingulate cortex.
The anterior cingulate cortex performs various functions, of which the most interesting for us are [10, p. 7183]: the conscious regulation of emotions through the re-examination of negative emotions, the suppression of excessive arousal and the suppression of the amygdala.
Those. when we understand that we are “ pounding ” in our fears, and we can consciously reject them, we must say thanks to our anterior cingulate cortex.
Prefrontal cortex

Fig. 13 . Prefrontal cortex.
The prefrontal areas of the cortex perform an important control function in the brain. These structures are necessary for arbitrary control. In addition, they participate in emotions and restrain involuntary impulsive reactions [19, p. 93]. The prefrontal cortex is involved in the decision-making process related to moral issues [31, p. 7],
human-conscious feelings arise when the signals of the limbic system reach the areas of the prefrontal cortex that support consciousness [31, p. 39].
The prefrontal cortex is the substrate for the main functions of the ego.[10, p. 7184], together with the amygdala, it controls an essential part of a person’s emotional life and provides adaptability. Disruption of this ligament can cause very acute emotional pain and darken human prudence.
Dorsomedial prefrontal cortex plays a central role in the implementation of downward cognitive modulation (ie, a person’s ability to analyze their feelings, evaluate their “ adequacy ” and, if necessary, suppress them) of fear and other emotions, perception of their emotional reactions and other people's emotional responses - the basis of mentalization and empathy . It is also the physiological basis for object relations [10, p. 7184].
While her activity is lowered, psychotherapy is not particularly effective [10, p. 7184] It is interesting that psychoanalysts, even in those times when visualization technologies were not invented, said that for a successful therapy a patient needs time to “strengthen the ego” (later it turned out that they meant increased activity of the dorsomedial prefrontal cortex).
This was achieved by creating a trusting, supportive relationship, validation, etc. Proper nutrition, rest and moderate exercise were also considered (and are considered) beneficial. Now for these purposes apply incl. antidepressants.
The signals of the prefrontal cortex can “block” pain, and this can be both a conscious and an unconscious process [31, p. 109]
Dorsolateral (not to be confused with dorsomedial, one lateral, the other - medial in spatial terms) prefrontal cortex is a key component of the infrastructure that provides executive functions of the psyche [10, p. 7184]: it relates to the processes of attention, concentration, effort control, operational memory and emotional memory.
The interaction between the amygdala and the prefrontal cortex is crucial for regulating the emotional response to environmental stimuli. [32, p. 6] It is believed that the medial prefrontal cortex regulates and controls the response of the amygdala to its stimuli [20, p. 115]
Orbitofrontal cortex
Technically, it is part of the prefrontal cortex .
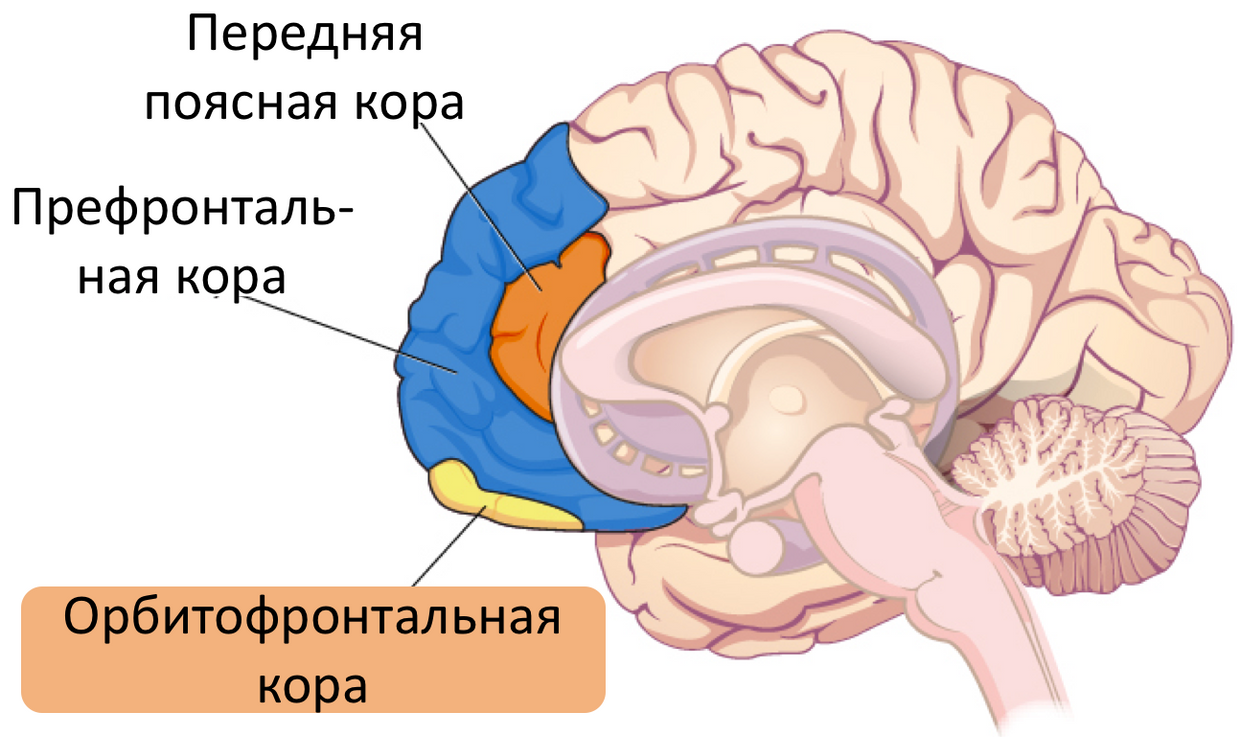
Fig. 14 . Orbitofrontal cortex.
The orbitofrontal cortex inhibits (or strengthens, depending on its condition) impulsive activity in each specific situation in response to the impact of certain kinds of stimuli ( sexual stimulation, risk, excitement ), and is also responsible for the manifestation of pronounced personality characteristics [10, p. 7186]
studies using imaging showed that the euphoria associated with the use of certain substances that correlates with an increase in metabolic activity in the orbitofrontal cortex and reticular formation, while as disf Oriya caused by abstinence, a decrease in activity in these zones [10, p. 7186].
This part of the brain is directly related to decision making [39]. According to the findings of neurobiologist Antonio Damasio [40], in the decision-making process people involve not only the cognitive, but also the emotional sphere: when faced with too complex (contradictory, in conditions of lack of data) choice, a person overloads his makeup, and she stops cope.
This is where the emotional sphere connects, just to make at least some decision, and the orbitofrontal cortex serves as a “ hub ” connecting the cognitive and emotional spheres.
It has been shown [35] that in patients with OCD, the volume of the orbitofrontal cortex of the left hemisphere is less than in healthy people.
On mental diseases in terms of neurophysiology and biochemistry
Now we will take a very brief look at exactly how the considered (and some other) components of the brain are related to mental illness and mental problems of healthy people. We will not consider here the whole nosology of mental illness (this is the topic of a separate large article), but briefly go over the most famous of them.
Depression
When depression reduced activity dorsolateral prefrontal cortex, thereby experiencing experience alone, social isolation and establishment of low productivity standards [10, p. 7185]
Depression is associated with a reduction in the interaction between mandelic and dorsal anterior cingulate cortex [32, p. 6]
Studies using imaging techniques have shown that the subgenual anterior cingulate cortex is excessively active in depression, and some treatments, such as antidepressants, electroconvulsive therapy and transkarnical magnetic stimulation leads to a decrease in activity in this area [10, p. 182].
Some evidence suggests that during depression, the volume of the hippocampus decreases [50].
Schizophrenia
So far, it has not been possible to establish specific and unambiguous connections between brain areas and schizophrenia, but at the moment this pathology is associated with changes in the hippocampus, entorhinal cortex , multimodal associative cortex, limbic system, tonsil, cingulate cortex, thalamus and medial temporal lobe [10 p. 239].
Obsessive compulsive disorder
Currently, there are two main ways to explain the pathophysiology of OCD: through the cortico-thalamic-cortical pathway and through the connection of the limbic system and the cortex [30].
Insel cites data [36] based on an analysis of studies using visualization, according to which OCD symptoms are explained by pathology in three regions of the brain: the orbitofrontal cortex, the cingulate cortex and (to a lesser extent) the caudate nucleus: excessive activity in the head portion of the caudate nucleus suppresses (inhibits ) transfer to the fibers of the white ball, which usually quenches the activity of the thalamus.
As a result, the thalamus increases the activity of the orbitofrontal cortex, which, through the cingulate cortex, closes at the head of the caudate nucleus, forming a cycle of positive feedback.
Early maladaptive schemes
In contrast to the above nosological units, the early non-maladaptive schemes themselves are not a mental illness: there is no such diagnosis.
However, it makes sense to include them in this article, since they are very widespread in healthy people and significantly hinder them.
What is the early maladaptive scheme (hereinafter - just a “ scheme ”)? A scheme is such a psychic construction that includes memories, thoughts, emotions, and body sensations. And they do not simply enter, but in a cunning manner are interconnected and interdependent [48, p. 41].
The scheme is formed somewhere in the early history of the life of an individual (usually in childhood, but maybe later) as a reaction to some events or phenomena of relationships with people significant for this person (the very "papa beat, mom didn’t like "). The
amygdala keeps unconscious information about trauma / negative emotional experience.
When a person encounters stimuli resembling events that led to the formation of a pattern, the amygdala triggers an unconscious process of activating those very emotions and physical sensations. faster than a person manages to understand anything.
When the circuit is activated, the person covers the wave of emotions and bodily sensations. It is not always aware of the connection with the lived experience of the original trauma.
Osozna aemye memories of trauma are stored in the hippocampus [48, p. 41] and the higher regions of the cortex. In fact, the emotional and cognitive aspects of traumatic experiences are stored in different parts of the brain.
Example of the scheme: a boy as a child climbed into his father's toolbox, his father brutally beat him. Many years have passed, the boy has grown and will present a certain project to customers. Everything is good with him - he copes with anxiety, he is thoroughly prepared, but here one of the listeners asks him a question ...
And the amygdala is activated (for example, from a tone or some characteristic word), launching the scheme. The speaker is unsettling this question, he begins to worry, forget details, feel incompetent, sweating, trembling, etc.
The task that is usually put in working with schemes is to strengthen the control of the prefrontal cortex over the amygdala.
Research results
Now that we have at least some understanding of how conversational therapy should affect the brain, and how this very brain works, it's time to talk about the results of research, the purpose of which was to evaluate the effect of psychotherapy on the morphological and biochemical characteristics of the brain.
In a meta-analysis [32], a significant relationship was found between the effect of therapy on the rostral anterior cingulate cortex and the precentral sulcus (increased activity), which more or less coincides with the initial assumptions.
The ventral rostral prefrontal cortex has extensive connections with brain regions responsible for processing emotions, in particular, with the amygdala. In addition, she participates in the decision-making process and the reward system.
In healthy people, the regulation of emotions is associated with the suppression of the activity of the tonsil by the rostral and dorsal cingulate cortex and some regions of the anterior cingulate cortex. Those. “Fear coming from the depths” in response to a stimulus at some point is intercepted, analyzed and “canceled.” Jugging on negative thoughts that is
characteristic of depression can be explained by a decrease in the level of connection between the cortical and amygdala. “ I am a loser ,” “ everything will be bad, ” etc. The increased activity of the rostral cingulate as a result of the use of psychotherapy may reflect improvements in emotional regulation and may be a possible basis for a cognitive reappraisal mechanism .
A cognitive revaluation is essentially one of the cornerstones of KPT. It lies in the fact that automatically arising negative thoughts to catch and analyze, and then replaced by more adequate (not containing cognitive distortion).
The increased activity of the anterior cingulate cortex is manifested after a course of CPT, and, after a course of long-term psychodynamic therapy, this activity decreases [32, p. 18].
However, the authors do not give any interpretations about this, and we will not invent a gag. Perhaps the point here is that in some studies the whole cortex is considered entirely, and in others the subgenual part of it (reduction in the activity of which correlates with a decrease in the feeling of guilt and oppression of repressed emotions).
Long-term verbal therapy leads to a decrease in activity in the left precentral gyrus , which is usually associated with motor functions, but may be involved in the processes of cognitive functioning.
A systematic study showed a weakening of the activity of the amygdala as a result of the use of CPT and psychodynamic therapy [32, p. 19]. And since the amygdala is the “center of fear” (again, a very, very figurative analogy), a decrease in its activity should lead to a decrease in the severity of depressive and anxious symptoms.
In another systematic meta-study [37], the authors concluded that anomalies in the hippocampus, amygdala, lower frontal gyrus, hookas well as in areas actively involved in managing emotions (dorsolateral prefrontal cortex and anterior cingulate cortex) are predictors of successful psychotherapeutic treatment of anxiety disorders.
Or, if one could fantasize a little, then with some stretch one can say that with successful treatment of anxiety disorders, changes in these areas will be observed.
In a study of the effects of psychotherapy in depression, it was shown [41] that conversational therapy leads to the normalization of the connections between the limbic system and the cortex, especially in the anterior cingulate cortex. In the same study, the use of islet fraction activity was suggested.as a biomarker that will help the doctor determine which treatment method is best suited in this particular case - psycho-or pharmacotherapy.
In a meta-study [42] of therapy by the method of desensitization and processing by the movement of the eyes (not quite colloquial therapy, the essence of which is to recall traumatic memories and move your eyes to and fro, no matter how funny it may sound), a change in the pattern of interaction between hemispheres.
It also presented data indicating an increase in the volume of the hippocampus, an increase in the activity of the anterior cingulate cortex, and the left frontal lobe. These and other data suggest that this therapy leads to increased control of the prefrontal cortex over the too active limbic system.
A study of the effects of long-term psychodynamic psychotherapy has shown that this treatment reduces the activity of the amygdala / hippocampus, subgenual cingulate cortex and medial prefrontal cortex [44]. These changes correlated with a decrease in the symptoms of depression.
How psychotherapy affects the brain
Well, research quite convincingly shows us that the brain changes under the influence of verbal therapy. But how exactly does he do it?
The answer lies in its such property as neuroplasticity. More precisely, not so: there is no direct evidence that psychotherapy increases brain neuroplasticity, but the common place is the idea that this very neuroplasticity is somehow involved in the process of psychotherapy [49].
As applied to the nervous system, neuroplasticity is the ability of nerve elements and regulatory molecules to adaptive reorganization under the influence of endogenous and exogenous influences [46, 79].
Neuroplasticity is observed at different levels [47] - at the level of the brain as a whole, at the level of its individual components, at the level of neurons, and even at the subcellular level.
The fundamental component of neuroplasticity is the plasticity of synaptic connections (ie, connections between neurons), which constantly disappear and reappear, and the balance of these opposite processes depends primarily on the activity of neurons [47].
The dependence of synaptic plasticity on activity is one of the central points of the concept of neuroplasticity, as well as theories of learning and memory, based on the experience of changes in the structure and function of synapses.
Long-term plasticity is realized as a result of changes in the expression of genes triggered by signaling cascades, which, in turn, are modulated by various signaling molecules with changes in neural activity.
A detailed examination of the molecular mechanisms of neuroplasticity is clearly beyond the scope of this article, so we will focus on the fact that the ability of the brain to change under the influence of external influences is proven. And it allows you to implement all those changes, which were discussed above.
Other factors affecting psychotherapy
Here we will talk about some additional hypotheses about exactly how therapy can affect the brain:
1. Perhaps psychotherapy affects the levels of neurotransmitters, in particular, serotonin . A review [49] showed that patients suffering from bipolar affective disorder and depression and who had lower serotonin levels (compared to the control group) in the prefrontal cortex and thalamus before the start of treatment showed an increase in serotonin levels in these areas after a year’s course of psychodynamic therapy. True, the study on the basis of which this conclusion was made has a less than ideal design (small sample, lack of successful reproduction).
2. It is possibletherapy affects the thyroid axis . The same review [49] refers to a study that showed that depressed patients who responded successfully to CPT achieved a reduction in T4 (thyroid hormone) levels, while patients who did not respond to therapy had it boost
3. Perhaps psychotherapy stimulates processes related to the neuroplasticity of the brain . As mentioned above, there is no clear evidence that psychotherapy leads to an increase in brain neuroplasticity, but there is evidence from animals, according to which training leads to it.
It is believed [49] that learning occurs through psychotherapy, which leads to an increase in the synaptic potentials of the neurons of the perforator path connecting the entorhinal cortex with the dentate gyrus of the hippocampal formation.
The same increase was demonstrated in animal models: rats that had undergone spatial orientation training had a greater density of dendritic spines compared with the two control groups.
Since the length of the dendrites, as well as the structure of their branching, remained unchanged, conclusions were made about the formation of new synapses.
Of course, directly transferring data from animal models to humans, and even taking into account different activities (direct learning in one case and psychotherapy in another) is not entirely correct, but some authors [49] consider it possible to use these data as an argument in the benefit of the hypothesis that psychotherapy alters the brain at the physical level.
Practical conclusions
Talking therapy can lead to significant changes in the brain. Naturally, not only is she - various mental exercises, meditation, and life experience in general, also use neuroplasticity to form the corresponding connectome.
However, studies show that during conversational therapy, these changes reach a higher level than in its absence.
The question of whether it is possible to use neuroplasticity for self-therapy, I will leave unanswered for the time being: the article turned out to be too long.
Video version
And here is the promised video version for those who prefer
Sorry for the quality of the broadcast, it's terrible, I know.
Literature
References
1. Recognition of psychotherapy effectiveness: The APA resolution. Campbell, Linda F.,Norcross, John C.,Vasquez, Melba J. T.,Kaslow, Nadine J. Psychotherapy, Vol 50(1), Mar 2013, 98-101. DOI: 10.1037/a0031817
2. Исурина Галина Львовна. Психотерапия и психологическое консультирование как виды клинико-психологического вмешательства // Медицинская психология в России. 2017. №3.
3. Stahl's Essential Psychopharmacology: the Prescriber's Guide. Stahl, Stephen M. MD, PhD / Softcover / Cambridge University Press / Pub Date 06/17 / 2017 / Edition 06 ISBN: 1316618137 — Subject Class: Pharmacology ISBN-13: 9781316618134
4. DeRubeis RJ, Hollon SD, Amsterdam JD, et al. Cognitive Therapy vs Medications in the Treatment of Moderate to Severe Depression. Arch Gen Psychiatry. 2005;62(4):409–416. doi:10.1001/archpsyc.62.4.409
5. Cuijpers, P., Sijbrandij, M., Koole, S. L., Andersson, G., Beekman, A. T. and Reynolds, C. F. (2013), The efficacy of psychotherapy and pharmacotherapy in treating depressive and anxiety disorders: a meta‐analysis of direct comparisons. World Psychiatry, 12: 137-148. doi:10.1002/wps.20038
6. Anthony P Morrison, Heather Law, Lucy Carter,Rachel Sellers,Richard Emsley, Melissa Pyle, Paul French,David Shiers, Alison R Yung, Elizabeth K Murphy, Natasha Holden, Ann Steele, Samantha E Bowe, Jasper Palmier-Claus, Victoria Brooks, Rory Byrne, Linda Davies, Peter M Haddad. Antipsychotic drugs versus cognitive behavioural therapy versus a combination of both in people with psychosis: a randomised controlled pilot and feasibility study. The Lancet Psychiatry. VOLUME 5, ISSUE 5, P411-423, MAY 01, 2018. DOI:https://doi.org/10.1016/S2215-0366(18)30096-8
7. Sagar V. Parikh, Zindel V. Segal, Sophie Grigoriadis, Arun V. Ravindran, Sidney H. Kennedy, Raymond W. Lam, Scott B. Patten. Canadian Network for Mood and Anxiety Treatments (CANMAT) Clinical guidelines for the management of major depressive disorder in adults. II. Psychotherapy alone or in combination with antidepressant medication, Journal of Affective Disorders, Volume 117, Supplement 1, 2009, Pages S15-S25, ISSN 0165-0327,https://doi.org/10.1016/j.jad.2009.06.042.
8. Siddique J, Chung JY, Brown CH, Miranda J. Comparative Effectiveness of Medication versus Cognitive Behavioral Therapy in a Randomized Controlled Trial of Low-income Young Minority Women with Depression. Journal of consulting and clinical psychology. 2012;80(6):995-1006. doi:10.1037/a0030452.
9. John G. Gunderson, M.D. With Paul S. Links, M.D., F.R.C.P.C. Borderline Personality Disorder. A Clinical Guide, Second Edition, 2008 — 366 pages. ISBN 978-1-58562-335-8
10. Sadock, Benjamin J., Virginia A. Sadock, and Pedro Ruiz. Kaplan & Sadock's comprehensive textbook of psychiatry. Philadelphia: Wolters Kluwer, 2017. Print.
11. Frankl, Viktor E. Man's search for meaning. Boston: Beacon Press, 2006. Print.
12. Beck, Aaron T. Cognitive therapy of depression. New York: Guilford Press, 1979. Print.
13. McWilliams, Nancy. Psychoanalytic diagnosis: understanding personality structure in the clinical process. New York: Guilford Press, 2011. Print.
14. Grof, Stanislav, Albert Hofmann, and Andrew Weil. LSD psychotherapy. Ben Lomond, Calif: Multidisciplinary Association for Psychedelic Studies, 2008. Print.
15. Falk Leichsenring (2005) Are psychodynamic and psychoanalytic therapies effective? A review of empirical data,The International Journal of Psychoanalysis, 86:3, 841-868, DOI:10.1516/RFEE-LKPN-B7TF-KPDU
16. Shedler, J. (2010). The efficacy of psychodynamic psychotherapy. American Psychologist, 65(2), 98-109. dx.doi.org/10.1037/a0018378
17. Leichsenring, F., & Rabung, S. (2011). Long-term psychodynamic psychotherapy in complex mental disorders: Update of a meta-analysis. British Journal of Psychiatry, 199(1), 15-22. doi:10.1192/bjp.bp.110.082776
18. Thomas Anstadt, Joerg Merten, Burkhard Ullrich & Rainer Krause (1997) Affective Dyadic Behavior, Core Conflictual Relationship Themes, and Success of Treatment, Psychotherapy Research, 7:4, 397-417, DOI: 10.1080/10503309712331332103
19. Мозг, познание, разум: введение в когнитивные нейронауки [Электронный ресурс]: в 2 ч. Ч. 1 / под ред. Б. Баарса, Н. Гейдж; пер. с англ. под ред. проф. В. В. Шульговского. — Эл. изд. — Электрон. текстовые дан. (1 файл pdf: 552 с.). — М.: БИНОМ. Лаборатория знаний, 2014. — (Лучший зарубежный учебник). — ISBN 978-5-9963-2352-4
20. Brozek, Bartosz, et al. The Emotional Brain Revisited. Place of publication not identified: International Specialized Book Services, 2014. Print.
21. Tryon, Warren W. Cognitive neuroscience and psychotherapy: network principles for a unified theory. Amsterdam: Elsevier Academic Press, 2014. Print.
22. Wheat, David & Hassan, Junaid. (2018). Capturing the Dynamics of a Psychiatric Illness: A System Dynamics Translation of the Contemporary Biological and Psychological Conceptualization of Panic Disorder (PD).
23. Николлс Джон, Мартин Роберт, Валлас Брюс, Фукс Пол. От нейрона к мозгу. / Пер. с англ. П.М. Балабана, А.В. Галкина, Р.А. Гиниатуллина, Р.Н. Хазипова, Л.С. Хируга. — М.: Едиториал УРСС, 2003. — 672 с. цв. вкл. ISBN: 5-354-00162-5
24. Jessica A. Grahn, John A. Parkinson, Adrian M. Owen, The cognitive functions of the caudate nucleus, Progress in Neurobiology, Volume 86, Issue 3, 2008, Pages 141-155, ISSN 0301-0082,https://doi.org/10.1016/j.pneurobio.2008.09.004.
25. Katrina L. Hannan, Stephen J. Wood, Alison R. Yung, Dennis Velakoulis, Lisa J. Phillips, Bridget Soulsby, Gregor Berger, Patrick D. McGorry, Christos Pantelis, Caudate nucleus volume in individuals at ultra-high risk of psychosis: A cross-sectional magnetic resonance imaging study, Psychiatry Research: Neuroimaging, Volume 182, Issue 3, 2010, Pages 223-230, ISSN 0925-4927,https://doi.org/10.1016/j.pscychresns.2010.02.006.
26. Rotge JY, Aouizerate B, Amestoy V, et al. The associative and limbic thalamus in the pathophysiology of obsessive-compulsive disorder: an experimental study in the monkey. Translational Psychiatry. 2012;2(9):e161-. doi:10.1038/tp.2012.88.
27.ocd.stanford.edu/about/understanding.html
28. Behrendt, Ralf-Peter. «Hippocampus and consciousness» Reviews in the Neurosciences, 24.3 (2013): 239-266. doi:10.1515/revneuro-2012-0088
29. Article Source: Hippocampus Is Place of Interaction between Unconscious and Conscious Memories
Züst MA, Colella P, Reber TP, Vuilleumier P, Hauf M, et al. (2015) Hippocampus Is Place of Interaction between Unconscious and Conscious Memories. PLOS ONE 10(3): e0122459.https://doi.org/10.1371/journal.pone.0122459
30. Jeste, Dilip V., and Joseph H. Friedman. Psychiatry for neurologists. Totowa, N.J: Humana Press, 2006. Print.
31. Carter, Rita, et al. The human brain book. New York, New York: DK Publishing, 2014. Print.
32. Sankar, A., Melin, A., Lorenzetti, V., Horton, P., Costafreda, S. G., & Fu, C. H. Y. (2018). A systematic review and meta-analysis of the neural correlates of psychological therapies in major depression. Psychiatry Research: Neuroimaging, 279, 31–39. doi:10.1016/j.pscychresns.2018.07.002
33. Brody, A. L., Saxena, S., Stoessel, P., Gillies, L. A., Fairbanks, L. A., Alborzian, S., … Baxter, L. R. (2001). Regional Brain Metabolic Changes in Patients With Major Depression Treated With Either Paroxetine or Interpersonal Therapy. Archives of General Psychiatry, 58(7), 631. doi:10.1001/archpsyc.58.7.631
34. Martin, S. D., Martin, E., Rai, S. S., Richardson, M. A., & Royall, R. (2001). Brain Blood Flow Changes in Depressed Patients Treated With Interpersonal Psychotherapy or Venlafaxine Hydrochloride. Archives of General Psychiatry, 58(7), 641. doi:10.1001/archpsyc.58.7.641
35. Kang DH, Kim JJ, Choi JS, et al. Volumetric investigation of the frontal-subcortical circuitry in patients with obsessive-compulsive disorder. J Neuropsychiatry Clin Neurosci. 2004;16:342–349.
36. Insel, T. R. (1992). Toward a Neuroanatomy of Obsessive-Compulsive Disorder. Archives of General Psychiatry, 49(9), 739. doi:10.1001/archpsyc.1992.0182009006
37. Santos, V. A., Carvalho, D. D., Van Ameringen, M., Nardi, A. E., & Freire, R. C. (2018). Neuroimaging findings as predictors of treatment outcome of psychotherapy in anxiety disorders. Progress in Neuro-Psychopharmacology and Biological Psychiatry. doi:10.1016/j.pnpbp.2018.04.001
38. Bloch, M. H., Leckman, J. F., Zhu, H., & Peterson, B. S. (2005). Caudate volumes in childhood predict symptom severity in adults with Tourette syndrome. Neurology, 65(8), 1253–1258. doi:10.1212/01.wnl.0000180957.98702.6
39. Antoine Bechara, Hanna Damasio and Antonio R. Damasio. Emotion, Decision Making and the Orbitofrontal Cortex. Cereb Cortex 2000; 10 (3): 295-307.
40. Damasio, A. (1991). Somatic Markers and the Guidance of Behavior. New York: Oxford University Press. pp. 217–299.
41. Rubart A, Hohagen F, Zurowski B. [Psychotherapy of Depression as Neurobiological Process — Evidence from Neuroimaging]. Psychother Psychosom Med Psychol. 2018 Jun;68(6) 258-271. doi:10.1055/a-0598-4972. PMID: 29864789.
42. Landin-Romero, Ramón & Moreno-Alcazar, Ana & Pagani, Marco & L. Amann, Benedikt. (2018). How Does Eye Movement Desensitization and Reprocessing Therapy Work? A Systematic Review on Suggested Mechanisms of Action. Frontiers in Psychology. 9. 10.3389/fpsyg.2018.01395.
43. Beutel, M. E., Stark, R., Pan, H., Silbersweig, D., & Dietrich, S. (2010). Changes of brain activation pre- post short-term psychodynamic inpatient psychotherapy: An fMRI study of panic disorder patients. Psychiatry Research: Neuroimaging, 184(2), 96–104. doi:10.1016/j.pscychresns.2010.06.005
44. Buchheim, A., Viviani, R., Kessler, H., Kächele, H., Cierpka, M., Roth, G., … Taubner, S. (2012). Changes in Prefrontal-Limbic Function in Major Depression after 15 Months of Long-Term Psychotherapy. PLoS ONE, 7(3), e33745. doi:10.1371/journal.pone.0033745
45. Etkin, A., Pittenger, C., Polan, H. J., & Kandel, E. R. (2005). Toward a Neurobiology of Psychotherapy: Basic Science and Clinical Applications. The Journal of Neuropsychiatry and Clinical Neurosciences, 17(2), 145–158. doi:10.1176/jnp.17.2.145
46. Олег Гомазков. Нейрогенез как адаптивная функция мозга. ИНСТИТУТ БИОМЕДИЦИНСКОЙ ХИМИИ ИМЕНИ В.Н.ОРЕХОВИЧА. М.: 2014.
47. Н.В. Гуляева. МОЛЕКУЛЯРНЫЕ МЕХАНИЗМЫ НЕЙРОПЛАСТИЧНОСТИ: РАСШИРЯЮЩАЯСЯ ВСЕЛЕННАЯ. БИОХИМИЯ, 2017, том 82, вып. 3, с. 365 – 371
48. Young, Jeffrey E., Janet S. Klosko, and Marjorie E. Weishaar. Schema therapy: a practitioner's guide. New York: Guilford Press, 2003. Print.
49. Liggan, Deborah Y., and Jerald Kay. “Some Neurobiological Aspects of Psychotherapy: A Review.” The Journal of Psychotherapy Practice and Research 8.2 (1999): 103–114. Print.
50. Arnone, D., McIntosh, A. M., Ebmeier, K. P., Munafò, M. R., & Anderson, I. M. (2012). Magnetic resonance imaging studies in unipolar depression: Systematic review and meta-regression analyses. European Neuropsychopharmacology, 22(1), 1–16. doi:10.1016/j.euroneuro.2011.05.003
2. Исурина Галина Львовна. Психотерапия и психологическое консультирование как виды клинико-психологического вмешательства // Медицинская психология в России. 2017. №3.
3. Stahl's Essential Psychopharmacology: the Prescriber's Guide. Stahl, Stephen M. MD, PhD / Softcover / Cambridge University Press / Pub Date 06/17 / 2017 / Edition 06 ISBN: 1316618137 — Subject Class: Pharmacology ISBN-13: 9781316618134
4. DeRubeis RJ, Hollon SD, Amsterdam JD, et al. Cognitive Therapy vs Medications in the Treatment of Moderate to Severe Depression. Arch Gen Psychiatry. 2005;62(4):409–416. doi:10.1001/archpsyc.62.4.409
5. Cuijpers, P., Sijbrandij, M., Koole, S. L., Andersson, G., Beekman, A. T. and Reynolds, C. F. (2013), The efficacy of psychotherapy and pharmacotherapy in treating depressive and anxiety disorders: a meta‐analysis of direct comparisons. World Psychiatry, 12: 137-148. doi:10.1002/wps.20038
6. Anthony P Morrison, Heather Law, Lucy Carter,Rachel Sellers,Richard Emsley, Melissa Pyle, Paul French,David Shiers, Alison R Yung, Elizabeth K Murphy, Natasha Holden, Ann Steele, Samantha E Bowe, Jasper Palmier-Claus, Victoria Brooks, Rory Byrne, Linda Davies, Peter M Haddad. Antipsychotic drugs versus cognitive behavioural therapy versus a combination of both in people with psychosis: a randomised controlled pilot and feasibility study. The Lancet Psychiatry. VOLUME 5, ISSUE 5, P411-423, MAY 01, 2018. DOI:https://doi.org/10.1016/S2215-0366(18)30096-8
7. Sagar V. Parikh, Zindel V. Segal, Sophie Grigoriadis, Arun V. Ravindran, Sidney H. Kennedy, Raymond W. Lam, Scott B. Patten. Canadian Network for Mood and Anxiety Treatments (CANMAT) Clinical guidelines for the management of major depressive disorder in adults. II. Psychotherapy alone or in combination with antidepressant medication, Journal of Affective Disorders, Volume 117, Supplement 1, 2009, Pages S15-S25, ISSN 0165-0327,https://doi.org/10.1016/j.jad.2009.06.042.
8. Siddique J, Chung JY, Brown CH, Miranda J. Comparative Effectiveness of Medication versus Cognitive Behavioral Therapy in a Randomized Controlled Trial of Low-income Young Minority Women with Depression. Journal of consulting and clinical psychology. 2012;80(6):995-1006. doi:10.1037/a0030452.
9. John G. Gunderson, M.D. With Paul S. Links, M.D., F.R.C.P.C. Borderline Personality Disorder. A Clinical Guide, Second Edition, 2008 — 366 pages. ISBN 978-1-58562-335-8
10. Sadock, Benjamin J., Virginia A. Sadock, and Pedro Ruiz. Kaplan & Sadock's comprehensive textbook of psychiatry. Philadelphia: Wolters Kluwer, 2017. Print.
11. Frankl, Viktor E. Man's search for meaning. Boston: Beacon Press, 2006. Print.
12. Beck, Aaron T. Cognitive therapy of depression. New York: Guilford Press, 1979. Print.
13. McWilliams, Nancy. Psychoanalytic diagnosis: understanding personality structure in the clinical process. New York: Guilford Press, 2011. Print.
14. Grof, Stanislav, Albert Hofmann, and Andrew Weil. LSD psychotherapy. Ben Lomond, Calif: Multidisciplinary Association for Psychedelic Studies, 2008. Print.
15. Falk Leichsenring (2005) Are psychodynamic and psychoanalytic therapies effective? A review of empirical data,The International Journal of Psychoanalysis, 86:3, 841-868, DOI:10.1516/RFEE-LKPN-B7TF-KPDU
16. Shedler, J. (2010). The efficacy of psychodynamic psychotherapy. American Psychologist, 65(2), 98-109. dx.doi.org/10.1037/a0018378
17. Leichsenring, F., & Rabung, S. (2011). Long-term psychodynamic psychotherapy in complex mental disorders: Update of a meta-analysis. British Journal of Psychiatry, 199(1), 15-22. doi:10.1192/bjp.bp.110.082776
18. Thomas Anstadt, Joerg Merten, Burkhard Ullrich & Rainer Krause (1997) Affective Dyadic Behavior, Core Conflictual Relationship Themes, and Success of Treatment, Psychotherapy Research, 7:4, 397-417, DOI: 10.1080/10503309712331332103
19. Мозг, познание, разум: введение в когнитивные нейронауки [Электронный ресурс]: в 2 ч. Ч. 1 / под ред. Б. Баарса, Н. Гейдж; пер. с англ. под ред. проф. В. В. Шульговского. — Эл. изд. — Электрон. текстовые дан. (1 файл pdf: 552 с.). — М.: БИНОМ. Лаборатория знаний, 2014. — (Лучший зарубежный учебник). — ISBN 978-5-9963-2352-4
20. Brozek, Bartosz, et al. The Emotional Brain Revisited. Place of publication not identified: International Specialized Book Services, 2014. Print.
21. Tryon, Warren W. Cognitive neuroscience and psychotherapy: network principles for a unified theory. Amsterdam: Elsevier Academic Press, 2014. Print.
22. Wheat, David & Hassan, Junaid. (2018). Capturing the Dynamics of a Psychiatric Illness: A System Dynamics Translation of the Contemporary Biological and Psychological Conceptualization of Panic Disorder (PD).
23. Николлс Джон, Мартин Роберт, Валлас Брюс, Фукс Пол. От нейрона к мозгу. / Пер. с англ. П.М. Балабана, А.В. Галкина, Р.А. Гиниатуллина, Р.Н. Хазипова, Л.С. Хируга. — М.: Едиториал УРСС, 2003. — 672 с. цв. вкл. ISBN: 5-354-00162-5
24. Jessica A. Grahn, John A. Parkinson, Adrian M. Owen, The cognitive functions of the caudate nucleus, Progress in Neurobiology, Volume 86, Issue 3, 2008, Pages 141-155, ISSN 0301-0082,https://doi.org/10.1016/j.pneurobio.2008.09.004.
25. Katrina L. Hannan, Stephen J. Wood, Alison R. Yung, Dennis Velakoulis, Lisa J. Phillips, Bridget Soulsby, Gregor Berger, Patrick D. McGorry, Christos Pantelis, Caudate nucleus volume in individuals at ultra-high risk of psychosis: A cross-sectional magnetic resonance imaging study, Psychiatry Research: Neuroimaging, Volume 182, Issue 3, 2010, Pages 223-230, ISSN 0925-4927,https://doi.org/10.1016/j.pscychresns.2010.02.006.
26. Rotge JY, Aouizerate B, Amestoy V, et al. The associative and limbic thalamus in the pathophysiology of obsessive-compulsive disorder: an experimental study in the monkey. Translational Psychiatry. 2012;2(9):e161-. doi:10.1038/tp.2012.88.
27.ocd.stanford.edu/about/understanding.html
28. Behrendt, Ralf-Peter. «Hippocampus and consciousness» Reviews in the Neurosciences, 24.3 (2013): 239-266. doi:10.1515/revneuro-2012-0088
29. Article Source: Hippocampus Is Place of Interaction between Unconscious and Conscious Memories
Züst MA, Colella P, Reber TP, Vuilleumier P, Hauf M, et al. (2015) Hippocampus Is Place of Interaction between Unconscious and Conscious Memories. PLOS ONE 10(3): e0122459.https://doi.org/10.1371/journal.pone.0122459
30. Jeste, Dilip V., and Joseph H. Friedman. Psychiatry for neurologists. Totowa, N.J: Humana Press, 2006. Print.
31. Carter, Rita, et al. The human brain book. New York, New York: DK Publishing, 2014. Print.
32. Sankar, A., Melin, A., Lorenzetti, V., Horton, P., Costafreda, S. G., & Fu, C. H. Y. (2018). A systematic review and meta-analysis of the neural correlates of psychological therapies in major depression. Psychiatry Research: Neuroimaging, 279, 31–39. doi:10.1016/j.pscychresns.2018.07.002
33. Brody, A. L., Saxena, S., Stoessel, P., Gillies, L. A., Fairbanks, L. A., Alborzian, S., … Baxter, L. R. (2001). Regional Brain Metabolic Changes in Patients With Major Depression Treated With Either Paroxetine or Interpersonal Therapy. Archives of General Psychiatry, 58(7), 631. doi:10.1001/archpsyc.58.7.631
34. Martin, S. D., Martin, E., Rai, S. S., Richardson, M. A., & Royall, R. (2001). Brain Blood Flow Changes in Depressed Patients Treated With Interpersonal Psychotherapy or Venlafaxine Hydrochloride. Archives of General Psychiatry, 58(7), 641. doi:10.1001/archpsyc.58.7.641
35. Kang DH, Kim JJ, Choi JS, et al. Volumetric investigation of the frontal-subcortical circuitry in patients with obsessive-compulsive disorder. J Neuropsychiatry Clin Neurosci. 2004;16:342–349.
36. Insel, T. R. (1992). Toward a Neuroanatomy of Obsessive-Compulsive Disorder. Archives of General Psychiatry, 49(9), 739. doi:10.1001/archpsyc.1992.0182009006
37. Santos, V. A., Carvalho, D. D., Van Ameringen, M., Nardi, A. E., & Freire, R. C. (2018). Neuroimaging findings as predictors of treatment outcome of psychotherapy in anxiety disorders. Progress in Neuro-Psychopharmacology and Biological Psychiatry. doi:10.1016/j.pnpbp.2018.04.001
38. Bloch, M. H., Leckman, J. F., Zhu, H., & Peterson, B. S. (2005). Caudate volumes in childhood predict symptom severity in adults with Tourette syndrome. Neurology, 65(8), 1253–1258. doi:10.1212/01.wnl.0000180957.98702.6
39. Antoine Bechara, Hanna Damasio and Antonio R. Damasio. Emotion, Decision Making and the Orbitofrontal Cortex. Cereb Cortex 2000; 10 (3): 295-307.
40. Damasio, A. (1991). Somatic Markers and the Guidance of Behavior. New York: Oxford University Press. pp. 217–299.
41. Rubart A, Hohagen F, Zurowski B. [Psychotherapy of Depression as Neurobiological Process — Evidence from Neuroimaging]. Psychother Psychosom Med Psychol. 2018 Jun;68(6) 258-271. doi:10.1055/a-0598-4972. PMID: 29864789.
42. Landin-Romero, Ramón & Moreno-Alcazar, Ana & Pagani, Marco & L. Amann, Benedikt. (2018). How Does Eye Movement Desensitization and Reprocessing Therapy Work? A Systematic Review on Suggested Mechanisms of Action. Frontiers in Psychology. 9. 10.3389/fpsyg.2018.01395.
43. Beutel, M. E., Stark, R., Pan, H., Silbersweig, D., & Dietrich, S. (2010). Changes of brain activation pre- post short-term psychodynamic inpatient psychotherapy: An fMRI study of panic disorder patients. Psychiatry Research: Neuroimaging, 184(2), 96–104. doi:10.1016/j.pscychresns.2010.06.005
44. Buchheim, A., Viviani, R., Kessler, H., Kächele, H., Cierpka, M., Roth, G., … Taubner, S. (2012). Changes in Prefrontal-Limbic Function in Major Depression after 15 Months of Long-Term Psychotherapy. PLoS ONE, 7(3), e33745. doi:10.1371/journal.pone.0033745
45. Etkin, A., Pittenger, C., Polan, H. J., & Kandel, E. R. (2005). Toward a Neurobiology of Psychotherapy: Basic Science and Clinical Applications. The Journal of Neuropsychiatry and Clinical Neurosciences, 17(2), 145–158. doi:10.1176/jnp.17.2.145
46. Олег Гомазков. Нейрогенез как адаптивная функция мозга. ИНСТИТУТ БИОМЕДИЦИНСКОЙ ХИМИИ ИМЕНИ В.Н.ОРЕХОВИЧА. М.: 2014.
47. Н.В. Гуляева. МОЛЕКУЛЯРНЫЕ МЕХАНИЗМЫ НЕЙРОПЛАСТИЧНОСТИ: РАСШИРЯЮЩАЯСЯ ВСЕЛЕННАЯ. БИОХИМИЯ, 2017, том 82, вып. 3, с. 365 – 371
48. Young, Jeffrey E., Janet S. Klosko, and Marjorie E. Weishaar. Schema therapy: a practitioner's guide. New York: Guilford Press, 2003. Print.
49. Liggan, Deborah Y., and Jerald Kay. “Some Neurobiological Aspects of Psychotherapy: A Review.” The Journal of Psychotherapy Practice and Research 8.2 (1999): 103–114. Print.
50. Arnone, D., McIntosh, A. M., Ebmeier, K. P., Munafò, M. R., & Anderson, I. M. (2012). Magnetic resonance imaging studies in unipolar depression: Systematic review and meta-regression analyses. European Neuropsychopharmacology, 22(1), 1–16. doi:10.1016/j.euroneuro.2011.05.003
