Direct comparison of laser myopia correction methods or what you pay for when choosing ReLEx SMILE
Here we “repaired” the Boomburum laser , and in a post where he talked about his new eyes, a discussion arose on the topic of comparing PRK methods, LASIK methods and SMILE methods. We (I mean the German holding SMILE EYES , which includes our Russian clinic) do all three types of operations, but are absolute supporters of the method that will give more if you lose less. Thus, any kind of LASIK or PRK is recommended only when SMILE is impossible: firstly, with farsightedness (this is a completely different story), and secondly, in cases of a diseased or damaged cornea (for example, with scars). But, of course, the economic side is taken into account.
It would seem that in the first posts I explained why. But in the comments to the post it is clear that this was not enough. Therefore, let's do everything according to the rules of scientific discussion. Let us analyze the theses and present the relevant studies to them.
This is what they do in the scientific and medical world. If there is an opinion, it needs to be justified. Preferably, in a sample of 20 or more patients with the same distribution in a double study. It is advisable that the studies be confirmed by different clinics in different countries where these types of operations are performed.
Let's start.
Define the terms
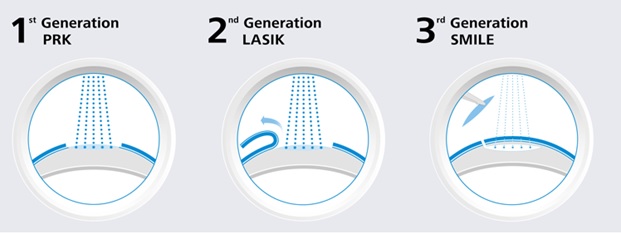
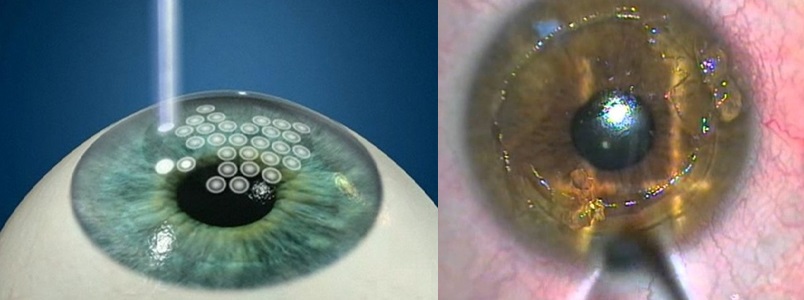
SMILE (ReLEx SMILE or simply SMILE) born in 2007 - Small incision lenticular extraction - 100% femtosecond technology. The Femto-prefix means that the laser has a very short pulse: 10 15 pulses fit in every second . In this case, the coherence and power of the outgoing beam is maximum. With its help, three-dimensional cutting of the “figure” takes place in the form of an individual lens - a lenticular inside the cornea and its removal through the small entrance (1.5 - 4 mm). The "figure" is extracted microinvasively from the inner layer of the cornea - nothing is evaporated, and the cornea takes on a new shape. Here are the details. Here is the principle of operation , and here the operation itself. Inside the SMILE EYES holding - 0.5% for enchancment (post-correction), in the world - up to 2%.

This is how ReLEx SMILE
FLEX born in 2005 is born - the predecessor of the SMILE method, also 100% femtosecond technology. Now it is fashionable to sell it as a “pseudo SMILE”. The difference is that, like SMILE, an individual lens is cut out in the cornea, but a cap-flap is cut out to circumferentially extract it. That is, there is no heating and evaporation - this is a plus, but otherwise - the same opening of the "cover". It is done under one laser, an excimer is not needed. It does not give the patient significant advantages over femtoLASIK. The equipment manufacturer offers it as part of preparing the surgeon for the SMILE method.
femtoLASIK (FS-LASIK, femtosecond LASIK) born in 2000 - a method using necessarily two lasers: a femtolaser and an excimer laser.
To form a “cap” in the cornea, a femtolaser is used, then the cap manually leans back. An excimer laser is needed to vaporize the lens in the middle layers of the cornea. There is a thermal effect. The operation depends on the quality of each of the two lasers (old models of either one or the other can spoil the overall result). Then the lid is placed in its original place. It never grows, you can always raise. The purpose of the operation is not to burn over the upper layers of the cornea, which are the most durable and contain the largest number of nerve endings. Now it is one of the most common operations in Russia and in the world. Inside the holding is only about 5-10% of the entire correction of myopia. Statistics on corrections in the world - 8-12%.
The term "SUPER-LASIK"- not a separate method - it is used as a characteristic of the evaporation profile by an excimer laser - it implies an individual profile of evaporation in the cornea. That is, it can be both “SUPER-femtoLASIK” and “SUPER-simply-LASIK”. In scientific medical publications, the term “Super Lasik” (namely with the prefix “Super”) is not used and is not an official medical term. It gained some distribution in advertising of some medical clinics, apparently wishing to draw additional attention to themselves due to “vivid terminology”.
Lasik(Laser-Assisted in Situ Keratomileusis) - born in 1989 - surgical department of the flap-cap using a microkeratome device, a special machine with a “shaving” blade and subsequent excimer laser evaporation of the lens on the cornea. To evaporate the lens in the middle layers of the cornea, one laser is needed - an excimer and a mechanical device with a microkeratome. LASIK - a combination of mechanical and laser exposure. The result depends on the quality of the laser and the quality of the microkeratome. There is a thermal effect.
All of its varieties are also morally obsolete: the Epi-LASIK technique - an attempt to reduce the thickness of the corneal section - indicates that the section is made on the very surface of the cornea and the REIK method- “radish horseradish is not sweeter” - this is the same LASIK. By the way, a thin flap “wrinkles” stronger and “flies” during an injury easier.
Also, the flap becomes the “culprit” of additional optical aberrations that affect the postoperative quality of vision.
In our clinic, today a microkeratome stands “sheathed” as an exhibit, for modern surgical practice it is already barbarism. It is extremely rarely needed, for example, to cut through scars.

Scheme LASIK / femtoLASIK
PRK (Photorefractive keratectomy, PRK) - born in 1985 - the method of evaporation of the lens in the upper layers of the corneal stroma without creating a flap with preliminary removal of the surface layer of the epithelium. The oldest method of all laser correction methods.
Complications are well studied, the largest statistics on them are up to 15%. Within 1-1.5 diopters of correction, it shows itself well, with higher myopia - all the shortcomings creep out. Due to complex healing, large wound surfaces and risks, it can only be recommended for economic reasons.
Of the minuses - the huge (πR2 - circle area!) Surface of the cornea “evaporates”, it is important that the strongest surface layers are destroyed, the border Bowman membrane is evaporated, the tissue evaporates exactly as much as with LASIK, scarring with the appearance of persistent opacities is possible - hiza.
The cornea of the eye has a layered structure: the epithelium, Bowman's sheath, stroma, descemet's sheath, posterior epithelium (endothelium). A stable refractive effect is achieved only when the geometry of the stroma (the main layer of the cornea) changes. Achieving stroma is a serious problem, therefore, all varieties of PRK differ in the way they pass through the first two layers: the epithelium and the Bowman's shell. In the old "classical" way, the epithelium was mechanically removed - scraped from the surface. There is a chemical exposure option with a 20% alcohol solution - and then scratch. Then it will be LASEK or epi-LASEK .
The epithelium can be "burned out" by the same excimer laser - it will be transepithelial PRK or Trans-PRK. In foreign publications, it is found under the designations "ASA", "ASLA", "C-Ten" and "TransPRK". In the early years, trans-PRK was a two-step procedure, in modern lasers it was a one-step procedure.
Therefore, it is correct to say that Trans-PRK is an improved technique, but only within the framework of this method - it allows to reduce a number of inevitable shortcomings of the PRK method itself and errors in the results.
But the method itself, alas, cannot be called new. Although even today there are clinics that sell Trans-PRK as the “most modern method”, and sometimes “the most sparing”. And the PRK - he is in Africa, the PRK, even if he is Trans. Marketing geniuses often do it great! For example, the Estonian procedure eLASIC, despite the name similar to another method, is PRK.
This is what the PRK looks like.
The only plus - all the same, there is no “cap” and related problems. Well, and one more thing - the surgeon does not need to bother by pressing the pedal twice and controlling the transitions from one software to another.
The appearance of the ReLEx SMILE method almost completely eliminated the need to perform PRK in any cases.
Our PRK technique is used solely for medical reasons in those cases where it is impossible to correct by other methods or if it is necessary to remove the upper layers of the stroma (for example, if there is clouding).
Here is a comparison of the entire line of methods.
SMILE versus PRK on a visual acuity scale
Research by Nethradhama Superspeciality Eye Hospital, doi: 10.1155 / 2017/5646390.
A sample of 120 eyes from 60 patients (34 women, 26 men) who underwent bilateral correction of mild myopia (up to 4 diopters) either using ReLEx SMILE or using PRK. Visual acuity, contrast sensitivity and higher order aberrations were recorded before surgery and compared after surgery. 3 months after surgery, a comparison was made.
Results: after 3 months, the SMILE group showed significantly better visual acuity compared to the PRK group. The postoperative spherical equivalent was comparable in both groups (SMILE = -0.15 ± 0.19 D, PRK = -0.14 ± 0.23 D, p = 0.72). However, the predictability of SE (spheroequivalent) was better in the SMILE group - 97% of the eyes within ± 0.05 D compared with 93% of the eyes in the PRK group.
General higher order aberrations were significantly higher in the PRK group compared to the SMILE group. SMILE showed slightly better contrast sensitivity. Four eyes from the PRK group lost one line of visual acuity due to blurring in the eyes.
Both SMILE and PRK are effective in correcting low myopia. However, the SMILE procedure offered better visual quality and better patient satisfaction due to greater postoperative comfort and lower induction of aberrations after 3 months.
My comment:when expanding the sample to 6 diopters, the PRK method would begin to lose numerically more, since it gives a much greater likelihood of turbidity (haze, haze) and subsequent blurring with increasing depth of cut. The structure of the cornea is restored after a serious burn of PRK with scars almost always, they often lie outside the visual region, at the borders of the lens evaporation and have little effect on visual acuity. However, this risk is crucial in the medical choice of a method for a healthy patient without special indications. Plus, in this study, patients noted a subjective quality of life higher in SMILE methods, since the postoperative period was painless (except for the first day).
By the way, the German refractive community Kommission Refraktive Chirurgie (KRC), as well as the German Association of Ophthalmologists (DOG), prohibits the use of PRK methods for correcting myopia by spheroequivalent more than -6 diopters. That is, if you have 5.5 and astigmatism more than 1.5, PRK cannot be done! In general, by choosing SMILE and saving the cornea, you minimize the recovery time.
But let's look at another study. It is more modern, therefore it was no longer compared PRK methods with SMILE, but more modern LASIK (which transmit much less energy to the eye, and to the middle parts of the stroma, and not to the skeleton) and SMILE. Here it is:
Corneal Transparency Assessment
Department of Ophthalmology, Philipps University of Marburg, Marburg, Germany, doi: 10.3109 / 02713683.2015.1107590
58 eyes with myopia from 33 patients treated with SMILE were compared with 58 eyes of 33 patients treated with FS-LASIK. All procedures were performed using a VisuMax femtosecond laser and an MEL 80 excimer laser. The result was evaluated by 3 optically significant concentric radial zones (0-2 mm, 2-6 mm and 0-6 mm) around the apex of the cornea and on 3 different anatomical corneal layers (front, center and rear).
After SMILE common, all layers of the cornea in a radial ring of 0-6 mm did not show significant changes compared with preoperative values. After FS-LASIK, the overall result was significantly reduced. 3 months after the operation, the results were leveled - there were no statistically significant differences between the two groups from all the studied annular spaces.
I translate the result: turbidity with SMILE does not immediately remain, and turbidity with femtoLASIK methods almost completely disappears in 3 months.
My comment: by the way, haze after PRK is visible decades later - like the scar marks after keratotomy. They look like this:

Hayes after PRK

Corneal
scars after radial keratotomy It is not yet possible to predict the tendency of the cornea to hase: the effect is due to the fact that the outer epithelium of the eye from the embryonic cells of the ectoderm (cornea) is separated by a Bowman’s membrane. When it is burned by PRK, a pseudo-Bowman membrane is visible on histology - this epithelium is in direct contact with the ectoderm cells and a skeleton begins to form to replace the lost membrane. This frame is not always transparent.
Bowman's membrane and haze - what is the danger of PRK (transFRK)
PRK (transFRK, etc.) is a cheap practical and well-studied method. But they left him for femtoLASIK methods, and then for SMILE. Why? Now I will try to explain this in simple words, and then I will show the research.
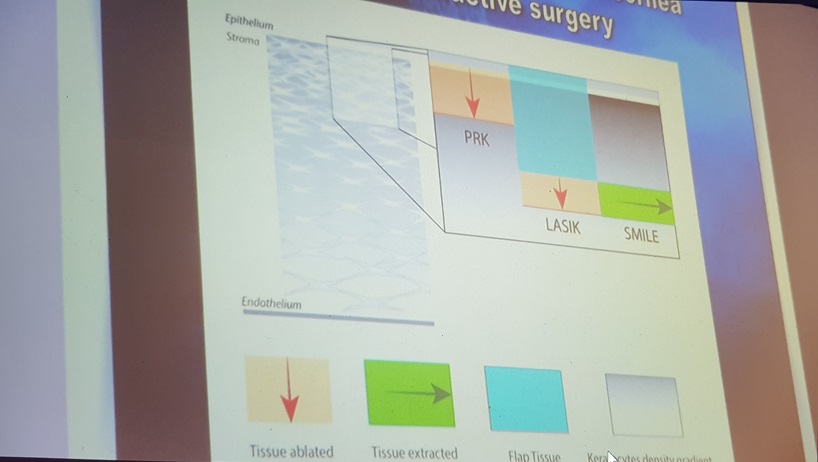
According to its morphology, the cornea as a pie consists of 5 layers: the epithelium, the anterior border (Bowman) membrane, its own substance (stroma), the posterior border (Descemet) membrane and endothelium.
At the stage of embryonic development, it is formed from three different types of tissue: the epithelium further develops from the surface ectoderm, the middle layer of the stroma from the mesoderm, and the inner layer of the endothelium from neuroectoderm. With the development and differentiation, each of these tissues needs to be isolated to maintain its structure and specificity, which is achieved by parallel development of the boundary membranes - the endothelium forms the Descemet shell, and the stroma forms the Bowman shell.
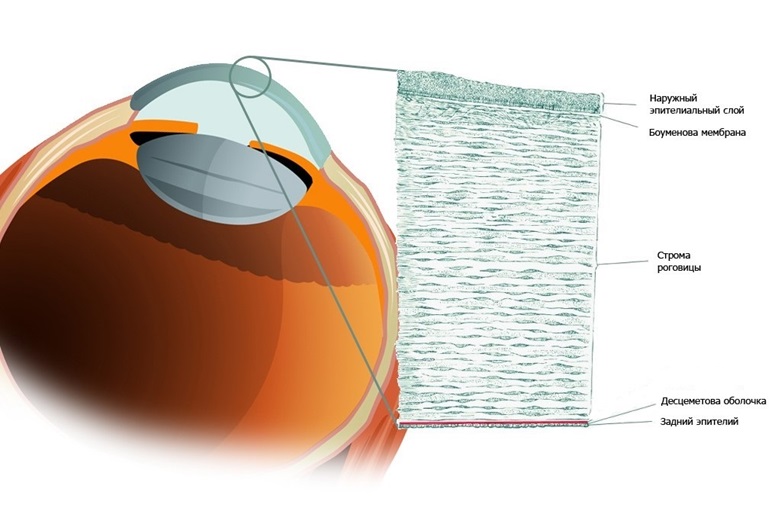
This is the structure of the cornea
. Normally, the cornea has physiological defects of the Bowman sheath, through which nerve fibers penetrate from the stroma into the epithelium. In a healthy cornea, there are few such openings, and there are certain protective mechanisms. When we evaporate the Bowman shell in PRK, we break the protective barriers and cause inflammation, the body reacts to this with the formation of fibrous connective tissue. Just subepithelial and intraepithelial fibrosis is haise (haise (fleur) - from the English. Haze - fog). It is the reason for the rather slow achievement of the final results when performing photorefractive keratectomy (PRK), this remains one of the main problems of the method. The stabilization of refraction, as a rule, lasts several months and may be accompanied by regression or the appearance of a chase.
Weakly treatable, pronounced turbidity, are rare. But even a transient moderate haze during its existence is able to reduce uncorrected visual acuity and contrast, which becomes a partial return to preoperative refraction and worsens the quality of life of patients.
Thus, the possible clouding of the cornea, the slow achievement of the optical effect and pain, make PRK (transFRK) one of the most unpopular methods of laser vision correction.
The traditional treatment after PRK involves the long-term use of corticosteroids, which allows to reduce the frequency and intensity of chyza, as well as to some extent affect the postoperative dynamics of refraction. However, in some cases, corneal opacities in the photoablation zone are quite persistent and intense, which requires a different approach to treatment. In this case, laser and even surgical methods can be added to drug therapy.
It should be noted that when using PRK as a way of post-correction, the risks are minimal, since the refractive component to be corrected is small. Especially in combination with surface treatment with antimetabolites. But with the primary correction of more than 1-2 diopters, all the deficiencies of the PRK are manifested with might and main.
Right herethere are details about the complications.
Nerves are restored, but it takes time. Therefore, after PRK methods, supportive therapy is needed (up to six months) so that nothing bad happens to the eye during this time. Complete regeneration to enough to manage the trophy level takes about a year. With the SMILE method, only about 10-15% of nerve endings are suppressed, which gives rise to significant differences.
The second feature is the corneal frame. By linkThere is a description of keratoconus - bulging forward of the cornea due to intraocular pressure. This is the most common complication, and it is extremely unpleasant. The only way to avoid it is to go deeper into the cornea. The cornea is heterogeneous. The most durable layers on the surface. At a depth of 120 to 150 microns, already loose layers begin. This is where work is done on all methods starting with LASIK. With PRK, we remove the strongest upper part of the stroma - see the picture above.
About the features of the fact that the epithelium and stroma are better kept separate, I already said. With PRK this is impossible, with other methods it is performed.
Aberration
"Comparison of the visual results after SMILE and femtosecond laser-assisted LASIK for myopia. Lin F, Xu Y, Yang Y. "
Sixty eyes from 31 patients with an average spherical equivalent of -5.13 ± 1.75 diopters underwent myopia correction using the SMILE procedure. Fifty-one eyes of 27 patients with an average spherical equivalent of -5.58 ± 2.41 diopters were treated using the FS-LASIK procedure. Results: no statistically significant differences in the parameters of visual acuity were found after either 1 or 3 months. High order aberrations and spherical aberrations were significantly lower in the SMILE group than the FS-LASIK group.
Conclusion: SMILE has a lower level of induction of higher order aberrations and lower spherical aberration than the FS-LASIK procedure.
My comment:The visual acuity after the femtosecond LASIK and after SMILE in quantitative terms was the same in the two groups, but the quality of vision in the group after SMILE was higher due to lesser induced aberrations.
This is due, firstly, to the fact that the SMILE profile is itself aspherical, and the creation of such a profile with an excimer is possible only on modern machines and requires 5-10% more corneal evaporation.
Secondly, the optical zone after SMILE is always slightly larger or equal to the planned one, and with a femtosecond LASIK it is slightly less than the planned one.
The damage factor, which is significant for femto and mechanical LASIK + exposure to an excimer laser, is completely absent with SMILE.
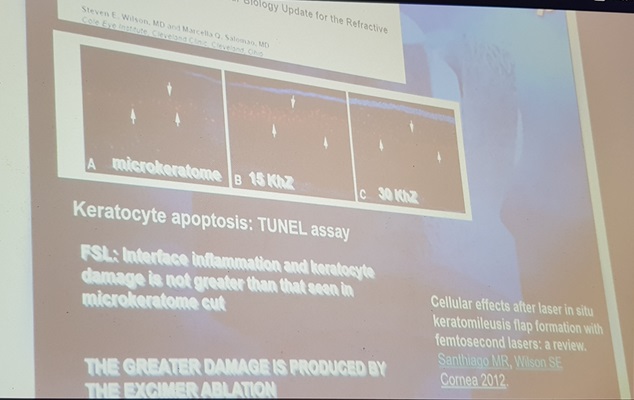
Comparison of biological indicators of corneal damage
According to the study "Comparison of Corneal Biological Healing After Femtosecond LASIK and Small Incision Lenticule Extraction Procedure" (doi: 10.3928 / 1081597X-20140320-03) on 128 eyes (69 for SMILE, 59 for femtoLASIK). Tests were made for visual acuity, refraction, the Norne test, the Schirmer test, the corneal sensitivity test, the ocular surface index, the corneal hysteresis, and the corneal stability coefficient were measured. Measurements were taken before the operation, on the first day, a week, a month, a quarter and six months after the operation. Result - there was no significant difference in the results for vision for SMILE and femtoLASIK. After surgery in the femtoLASIK group, the sensitivity of the cornea was significantly reduced, slightly changed in the SMILE group. The biological healing of the cornea after SMILE surgery in the early period exceeded femtoLASIK.
My comment: in patients after SMILE, dry eye syndrome is significantly less pronounced, corneal sensitivity and strength are preserved with comparable indicators of postoperative visual acuity.

Schirmer test (for tear production) and its result

Norn test (resistance of the tear film)
Now the next study.
Biomechanical properties of the human cornea
doi: 10.1007 / s10792-017-0575-6
In this experimental study, 11 pairs of human corneas unsuitable for transplantation were divided into two groups. The corneas of the right eye were treated with a femtosecond laser LASIK (FSLASIK), and the corneas of the left eye were treated with low-cut lenticular extraction (SMILE). Pachymetry was measured in each eye immediately before laser refractive surgery. All corneas underwent refractive correction of the –10.00 D and –0.75 D spheres of the cylinder at 0 ° with a 7 mm region, either with a 110 μm flap (FS-LASIK) or with a cap of 130 μm (SMILE). For two-dimensional biomechanical measurements, corneoscleral discs were subjected to two test cycles (preliminary strain curve from 0.03 to 9.0 N and stress relaxation at 9.0 N for 120 seconds) to analyze the properties of elastic and viscoelastic materials. The effective modulus of elasticity was calculated. Statistical analysis was performed with a confidence interval of 95%.
When measuring strain-strain, the effective elastic modulus was 1.47 times higher. The size of the effect is significant. No significant differences were observed among relaxation-stress measurements with an average remaining stress of 181 ± 31 kPa after SMILE and 177 ± 26 kPa and after FS-LASIK after relaxation.
Conclusions: Compared to a flap-based procedure such as FS-LASIK, the SMILE technique can be considered superior in terms of biomechanical stability when experimentally measured ex vivo on paired human eyes.
My comment: before that, the same results were calculated by mathematical modeling by Professor Ranstein (Great Britain), and Professor Secundo confirmed the theoretical conclusions by measuring on paired human eyes (his corneal strength after SMILE is even higher than in theory) in a special Swiss laboratory. These are truly revolutionary results!
So,
So what is better with myopia?
Let's go through the points again:
- The operations of PRK, femtoLASIK and SMILE are neither better nor worse than each other, each has its own field of application. It is logical to use PRK as a method of additional correction for special medical purposes. For the primary correction is not worth considering. FemtoLASIK can be made if there is no technological or financial opportunity to make SMILE, and the thickness and shape of the cornea allow you to cut the lid. ReLEx SMILE is the most gentle operation, the operation of choice in myopia and / or myopic astigmatism. It combines the advantages of two predecessor technologies - FemtoLASIK and PRK, but is devoid of their disadvantages.
- The PRK method (trans-PRK) destroys the outer epithelium of the eye, the Bowman membrane and the upper (most durable) layers of the cornea. On the downside, there is a violation of innervation (and dry eyes), opacities during the formation of a pseudoboumen membrane, average risks of keratectasia (protrusion of the cornea). In pluses - the ability to carry out this operation several times. PRK is certified in many countries for active sports.
In short, cool for those who love oldstyle technology - ready to change the new Mercedes to the old Volga GAZ-21. - FemtoLASIK suppresses about 75-90% of the superficial nerve endings in the cornea, the remaining barely enough to manage trophic, but this is better than burning the entire surface. The work is carried out in loose layers of the cornea, the frame suffers due to a cut of the lid. Due to the risk of displacement or detachment of the flip, it is not allowed for correction in a number of dangerous professions and for athletes. If everything went smoothly, it gives a good optical effect and accurate correction.
- SMILE - the most modern method, clinical use for more than 10 years: the first patients (except test pigs) have been walking after surgery since 2007. The corneal framework will remain, about 80% of the nerves are preserved. For use, you need a unique VisuMax laser and a well-trained surgeon to extract the cut material through a narrow tunnel. The most painless operation that allows you to use your eyes from the next day without restrictions - this determines its cost. It gives the least amount of distortion due to aberrations. About two million surgeries have now been performed worldwide, but the number of devices, clinics and operated patients is growing exponentially.
- Laser methods of vision correction are not the only possible methods of surgical vision correction: you can integrate lenses in the eye, segments in the cornea or replace your own lens with an artificial lens with new optical properties (more here ).
- Vision correction - in most cases, it is done because of a desire to improve the quality of life, rarely for medical reasons. Insurance medicine in most countries (including Russia) does not cover the costs of its implementation. It is up to you to do vision correction or wear glasses / contact lenses, but in any case, you need to be information-savvy to choose the right option.
I suggest you decide, using the facts.
