Why is it so difficult to continuously measure glucose levels?
- Transfer

Everyone starts the day with a routine, and like most modern people, I start by checking my phone. But if most people check the weather, traffic jams or Twitter and Facebook, I look at the phone a couple of centimeters inside my daughter's abdomen. There is a tiny electrochemical sensor that constantly monitors the intercellular fluid, measuring the concentration of glucose so that we can monitor the amount of insulin it receives through an insulin pump.
Type 1 diabetes is an unpleasant disease, usually attacking the victim at an early age, and transforming every day into a sequence of medical procedures — counting the right amount of insulin for use with each piece of food, working with the inevitable high and low glucose levels, and regular injections for testing blood. Continuous monitoring of glucose (NMG) has become manna from heaven for millions of diabetic families, as it allows us to allow our children to be children, let them go overnight and allow them to eat another slice of pizza without making it a scientific project. In addition, good glucose control means reducing the likelihood of the onset of the dangerous effects of diabetes in adulthood — blindness, heart disease, amputations. Also pretty cool
But with all the advantages of NMG it has its drawbacks. It is extremely expensive in terms of consumables and electronics, it requires an invasive procedure for installing sensors, and even in the era of tiny electronics it is relatively large. It would seem that we should have moved much further with all our technologies - but it turns out that it is quite difficult for NMGs to implement, and there are convincing reasons for making technology development stuck in place.
Sensor
NMG consists of three main components: the sensor itself, which converts the concentration of glucose in the body into an electrical signal; a transmitter that processes the signal and encodes it for wireless transmission; and a receiver, which can be a separate device, or be integrated directly into the insulin pump, and demonstrate the readings and graph of glucose change over the last 24 hours.
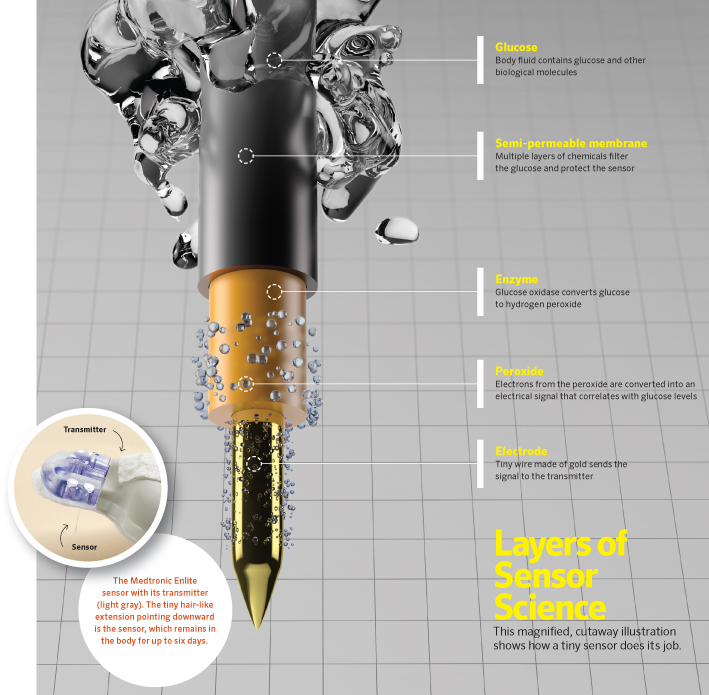
The key to everything is the sensor. His chemistry is simple: super pure gold wire is coated with glucose oxidase., an enzyme derived from the bacteria Penicillium notatum. This enzyme oxidizes β-D-glucose to glucono-1,5-lactone, which spontaneously hydrolyzes to gluconic acid. This forms hydrogen peroxide. Peroxide is oxidized on the gold wire, and the resulting current is proportional to the concentration of glucose in the interstitial fluid. The current is read by the system and used to calculate an estimate of blood glucose concentration based on a calibration curve.
But, although chemistry is simple, the difficulties of human biology and production complicate the task of practical use of the LMWH sensor. First, the sensors need to be inserted into the interstitial fluid, and left there for several days (although many stretch this period to save on the sensors). A foreign object in the body, a wire coated with proteins derived from bacteria, provokes the immune system, which is sharpened to combat such invasions. Without protection, the glucose oxidase that makes the sensor work will be destroyed by the immune system within a few hours. Therefore, the sensor requires special proprietary coatings that allow glucose to pass through but do not allow the immune system to attack the enzyme for some time.
The second difficulty is the processing of tiny components and the assembly of an interface for the transmitter, which digitizes the signals from the sensor and transmits them wirelessly to the receiver. The interface should provide both a place to connect the transmitter, and reliable skin grip, allowing it to stay there for weeks without provoking contact dermatitis or other side effects. Also, the sensor must somehow be combined with its input device, with a thick hypodermic needle, through which the thin wire of the sensor can pass without folds. The final assembly, of course, must be sterilized, so it must withstand radiation — the most common method of sterilizing medical devices.
Transmitter

My collection of dead transmitters, including the one that I opened. However, the transmitter that my daughter is currently using, they are pulling at $ 5,000, which the insurance does not pay.
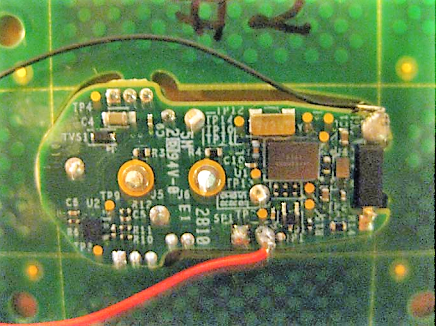
Considering all this, paying $ 75 for each NMG transmitter does not seem unreasonable. Questions about the cost I have in connection with the transmitters. Different manufacturers make different schemes, and even for one manufacturer, new technologies replace old ones. Of course, the scheme is difficult to get, but in the FCC ID database , as well as in the articles of annoyed usersit can be seen that the basic transmitters intestines are approximately what could be expected from any wireless technology - sensor signal processing, microcontroller, power management and wireless subsystem. We are now using 2.4 GHz ISM transmitters; Once we used Bluetooth transmitters, but they work four times less in time.
$ 600 for it ? Seriously?
Studying reviews with disassembling equipment, it is difficult to call a fair amount of $ 600, which I pay for each transmitter. We all know how little it costs to make such a device - probably no more than $ 5 apiece, and that will be generous. And yes, I know that I pay not for the components and labor of workers, but for the billions spent on research, development and clinical trials that were required to bring devices to the market. But I can't help thinking that there must be a better way.
The main problem is that the transmitters are sealed. Moreover, it is very hermetic, which is why it cannot be opened without breaking. And since it cannot be opened when the batteries are exhausted, you have to change it completely. This, of course, did not stop fearless hackers from trying to replace batteries. I have not tried it yet, but I put it on the list for the future. After opening the battery sensor, it is quite easy to replace the battery, but it is rather difficult to close it again, restoring water resistance.
In the blink of an eye

Prototype contact lenses for NMH from Verily
Should this go on and on? Is it really necessary to mess around with a relatively large, overall transmitter? It seems to me that it could be smaller and cheaper if it used RFID technology. An external transmitter could interrogate the sensor and receive a piece of data needed to encode the voltage on the sensor. Apparently, this way they were going to enroll in the company Verily, a manufacturer of medical devices owned by Google, which developed contact lenses for GPS. The idea seemed sensible, because glucose falls into tears, and leads to one of the early symptoms of type 1 diabetes - blurred vision due to sugar crystals falling on the cornea. Contact lenses definitely would not have a power source, so power had to be supplied from the outside.
Unfortunately, Verily has just announced that it is completing a project on contact lenses for LMWHs, since the biological obstacles to the collection of diagnostically useful and stable readings were too great. As we saw, NMG is not an easy thing, but something I can not believe that Verily abandoned the project only for technical reasons. My inner cynic says that the prospect of going through all the endless rounds of approvals turned out to be too unbearable - and this is a shame (pardon the pun) is a shame, given the breakthrough nature of the technology. However, it is very difficult to fight with already existing players who have already received all permissions, and even with deep pockets.
And yet I hope that someone else will take on the challenge of developing an improved version of the NMG. And now she is not bad, and I, of course, will do everything possible so that my child will continue to remain a cyborg. It is unfortunate that companies associated with NMGs know this and don’t feel the need to become generous when setting prices on the market they own.
