Human Immune System: Biological Antivirus. Antivirus databases
I apologize for the unrealistically huge break after the first part :(
Link to the first part (innate immunity)
So, something that penetrated the body was recognized as hostile and destroyed. But each time to identify extraneous entities by common non-specific signs is far from an optimal concept of behavior, since pathogens can develop a masking system that will prevent their detection.In order to detect these microorganisms (as well as increase the effectiveness of the response in relation to everyone else), a special specific (it is also acquired) immune system, which includes T-lymphocytes and B-lymphocytes, producing antibodies,
Formation and arrangement of antiviral bases of
T-cells.
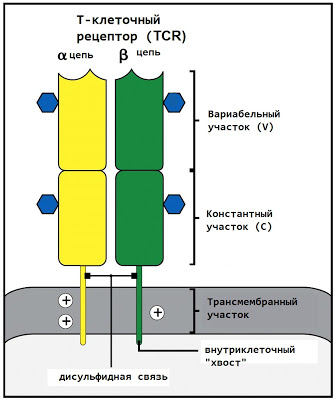
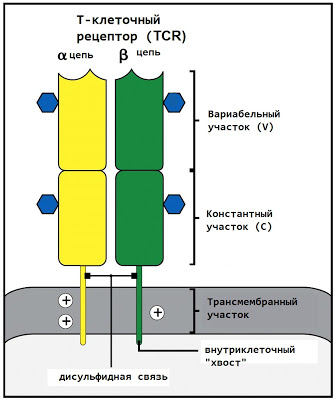
T-lymphocytes can recognize foreign agents using T-cell receptors (TCR - T cell receptor) - special protein molecules located on the surface of the cell. These receptors are not able to interact with foreign proteins directly - they require that the protein fragment be attached to the main histocompatibility complex (MHC) molecule described in the previous part. Why such a seemingly strange solution has been worked out will be explained below.
The T-cell receptor consists of two peptide chains (α and β), each of which is located at one end in the cytoplasm of the cell and can send signals deep into the cell, and the other (which will be discussed) in the intercellular space.
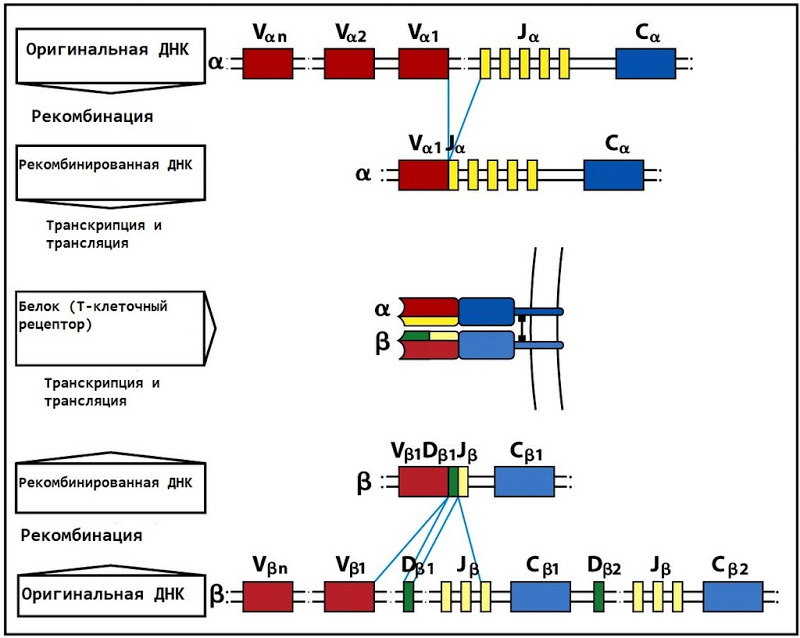
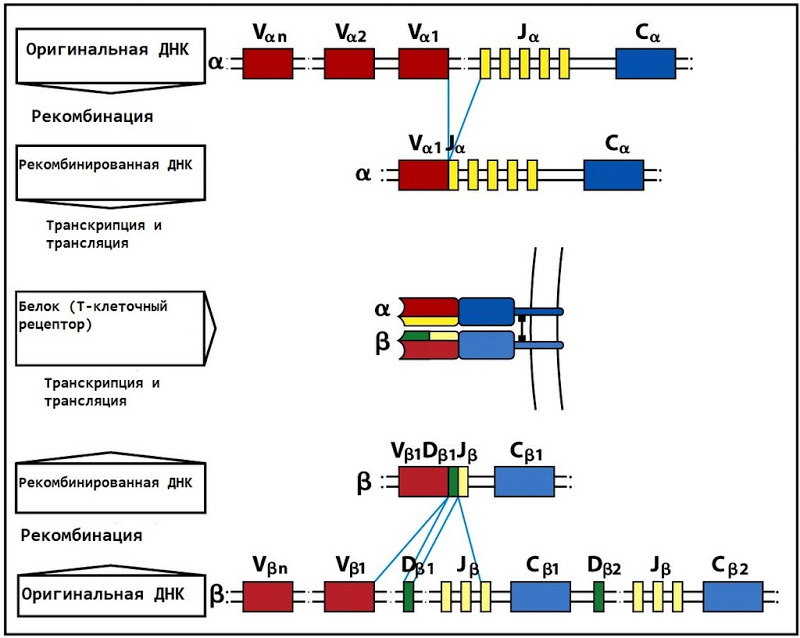
The outer end of each of the TCR chains consists of two fragments - variable (V) at the end and constant (.C) closer to the membrane. The constant region is the same in all human T-lymphocytes, while the variable region can vary.
The variable region is encoded by two (for the α-chain - V and J) or three (for the β-chain - V, D and J) DNA sections. Moreover, there are more than 50 different V fragments, 2 D and an average of 40 (13 for α and 61 for β) J fragments in the genome. When a T cell is formed in the bone marrow, the V, D, and J fragments are randomly selected from the existing heap. In addition, there are several more subtle mechanisms for introducing entropy, so after all this, the total number of possible TCR is about 10 ^ 18.
Thus formed T-cells leave the bone marrow and are sent to the thymus, where they will be finely adjusted to existing antigens. At this stage, lymphocytes are not yet active, as randomly formed receptors can threaten surrounding tissues.
Fine tuning in the thymus goes immediately in several directions. The first of these is positive selection. T cells try to interact with the antigen presenting cells (APCs) located there, on the surface of which there are MHC molecules. If the T cell is not able to adhere to the MHC, such a cell will not divide. If it can, such a cage will produce offspring.
The second is negative selection. In the thymus, proteins are produced from the entire body (including, for example, insulin), however, in scanty amounts - just to present them on the surface of the APC. If a T cell recognizes such a protein, it is immediately destroyed; an error in the eradication process usually leads to autoimmune diseases (in the case of insulin, to type 1 diabetes).

Now it should begin to become clear why T cells need MHC. The process of the first contact of a T-cell with an antigen must be controlled, otherwise it may begin to pose a threat to body tissues.
Thus, from a heap of randomly formed T cells, positive and negative selection results in a set of lymphocytes that are able to recognize proteins attached to MHC and safe for their own tissues. After that, these cells are sent to the lymph nodes, where they are activated.
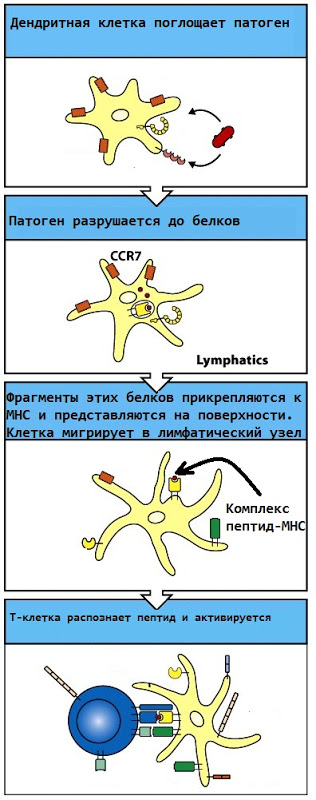
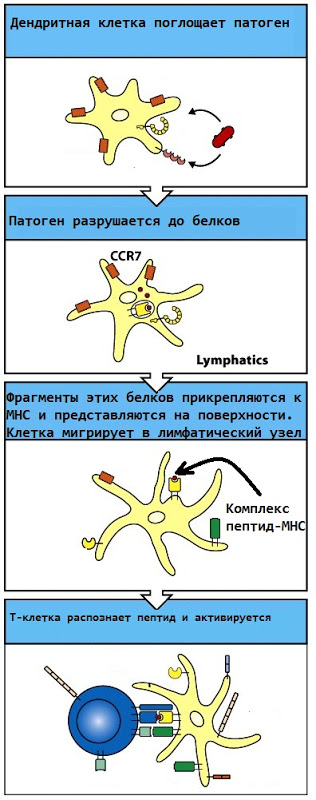
Activation of T-lymphocytes is the process after which these cells become able to actually perform their functions (destroy cells infected with the virus or activate B-cells and macrophages). In the lymph node there is a huge number of dendritic cells that absorb the infectious agent at the site of infection, break it down into proteins and present the corresponding proteins on its surface. After that, if the T-lymphocyte is able to recognize this protein (that is, its receptor is suitable for it), the T-lymphocyte “turns on”. Thus, only those lymphocytes that truly recognize a foreign protein are active.
After activation, T-lymphocytes are able to divide (clonal expansion), and freshly created copies of the lymphocyte in place are activated and enter the bloodstream or move to another area of the lymph node and there are responsible for the activation of B-cells.
B cells
Oddly enough, in general, they are quite similar to T lymphocytes. The main recognition tool, the B-cell receptor, is essentially an antibody attached to the surface of the cell. So let's look at the structure of the antibody.
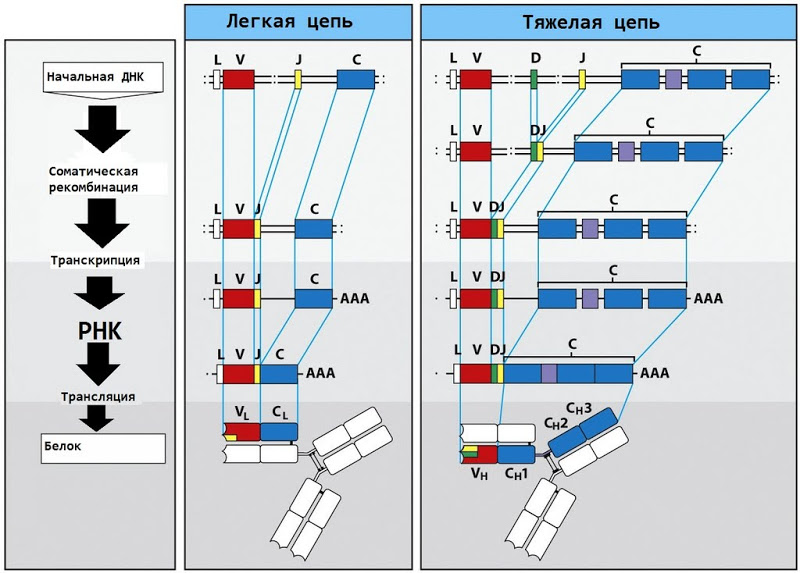
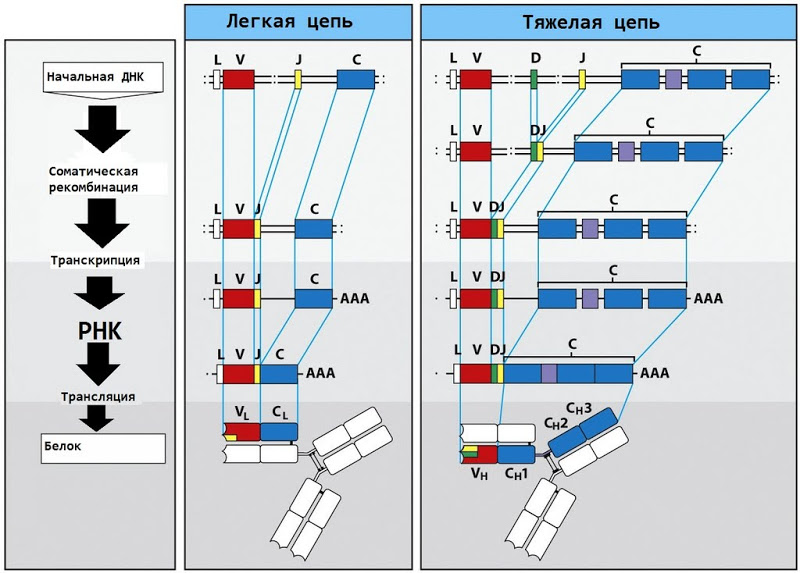
The basic IgM antibody (immunoglobulin M) consists of two heavy chains and two light chains; each light chain, like the chains of the T cell receptor, consists of a variable and constant region.

The variable region entropy generation mechanism is again similar to the TCR mechanism. There are 40 possible V fragments and 5 possible J fragments, which, if you add a number of random mutations to them, produce a huge number of different possible antibodies.
The fundamental difference between T- and B-lymphocytes lies in the mechanism of selection and activation. B cells do not undergo typical positive and negative selection. To avoid the threat of auto-activity, B-lymphocytes use T-cell selection.
After leaving the bone marrow, B-cells are sent directly to the lymph nodes. On the way, they can capture some proteins with their receptors, absorb them and present them bound to the MHC molecule on their surface.
To activate the B-cell, it is necessary to interact with the T-cell. With this interaction, the T-lymphocyte recognizes the MHC-protein complex on the surface of the B-lymphocyte and, if recognition occurs, activates the B-lymphocyte. It is not difficult to notice that ineffective or autoreactive B cells simply will not be activated, since the T lymphocytes that could do this were removed in the process of negative selection or were not activated.

After activation, the B-cell goes through a process called somatic hypermutation. It begins to divide frequently, and with each division, new mutations are introduced into the region of DNA that encodes the variable region of the antibody. Obviously, B cells that better recognize the antigen will be more frequently and actively activated, and we get ... That's right, normal natural selection. Which ultimately creates B cells, the antibodies of which ideally recognize some kind of antigen.
Ultimately, a B-lymphocyte becomes a plasma cell, which begins to produce antibodies on an industrial scale, and after the threat has passed, it becomes a memory cell that can produce suitable antibodies after a significant period of time.
Thus, the generation of “anti-virus databases” of the human body occurs randomly, however, only those signatures that have shown their effectiveness on pathogens that have already been recognized by heuristic mechanisms become active and are actually used.
The "friend or foe" system. The role of MHC
Unlike macrophages - professional phagocytes that simply devour pathogens, lymphocytes are capable of this, this is not their function. B cells exert their influence by secreting antibodies, and T cells by interacting with other cells.
All T-cells can be divided into three types: T-killets, T-helpers and T-suppressors. I will try to talk about T-suppressors in one of the following parts.
T-killers are designed to destroy pathogens (viruses or bacteria) that are inside the cells. For these purposes, in addition to TCR, they carry adjacent CD8 molecules on the surface, and together TCR and CD8 recognize type I MHC molecules.
MHC I are produced on the surface of every cell in the body. In their absence, the cell is killed by a natural killer (NK cell). All proteins that are inside the cell attach to MHC I. T-killer does not respond to any of them (due to negative selection). However, if a pathogen appears inside the cell, it will also be presented on the surface and will most likely be recognized by the T-killer, and the cell, along with the muck that is inside, will be destroyed.
MHC II is a different case. They are found only on the surface of APC - antigen-presenting cells (these are macrophages, dendritic cells and B cells), and T-helpers recognize them using CD4 molecules similar to CD8.
If proteins that are in the cytoplasm of the cell attach to MHC I, then proteins that were absorbed by the cell from the outside attach to MHC II. Thus, the proteins on the surface of APC are a kind of board “they are being searched for”. T-helpers first activate themselves after contact with a dendritic cell, and then activate B-cells (which begin to produce antibodies) and macrophages (which begin to more actively devour bacteria).

The resulting system is able to recognize the majority of infectious agents, both those that live between cells and intracellular. In addition, she does not spend extra energy on copying obviously inefficient cells and does not attack her own tissues.
Many thanks for the attention and bottomless respect to those who were able to read this heavy text to the end :)
Link to the first part (innate immunity)
So, something that penetrated the body was recognized as hostile and destroyed. But each time to identify extraneous entities by common non-specific signs is far from an optimal concept of behavior, since pathogens can develop a masking system that will prevent their detection.In order to detect these microorganisms (as well as increase the effectiveness of the response in relation to everyone else), a special specific (it is also acquired) immune system, which includes T-lymphocytes and B-lymphocytes, producing antibodies,
Formation and arrangement of antiviral bases of
T-cells.
T-lymphocytes can recognize foreign agents using T-cell receptors (TCR - T cell receptor) - special protein molecules located on the surface of the cell. These receptors are not able to interact with foreign proteins directly - they require that the protein fragment be attached to the main histocompatibility complex (MHC) molecule described in the previous part. Why such a seemingly strange solution has been worked out will be explained below.
The T-cell receptor consists of two peptide chains (α and β), each of which is located at one end in the cytoplasm of the cell and can send signals deep into the cell, and the other (which will be discussed) in the intercellular space.
The outer end of each of the TCR chains consists of two fragments - variable (V) at the end and constant (.C) closer to the membrane. The constant region is the same in all human T-lymphocytes, while the variable region can vary.
The variable region is encoded by two (for the α-chain - V and J) or three (for the β-chain - V, D and J) DNA sections. Moreover, there are more than 50 different V fragments, 2 D and an average of 40 (13 for α and 61 for β) J fragments in the genome. When a T cell is formed in the bone marrow, the V, D, and J fragments are randomly selected from the existing heap. In addition, there are several more subtle mechanisms for introducing entropy, so after all this, the total number of possible TCR is about 10 ^ 18.
Thus formed T-cells leave the bone marrow and are sent to the thymus, where they will be finely adjusted to existing antigens. At this stage, lymphocytes are not yet active, as randomly formed receptors can threaten surrounding tissues.
Fine tuning in the thymus goes immediately in several directions. The first of these is positive selection. T cells try to interact with the antigen presenting cells (APCs) located there, on the surface of which there are MHC molecules. If the T cell is not able to adhere to the MHC, such a cell will not divide. If it can, such a cage will produce offspring.
The second is negative selection. In the thymus, proteins are produced from the entire body (including, for example, insulin), however, in scanty amounts - just to present them on the surface of the APC. If a T cell recognizes such a protein, it is immediately destroyed; an error in the eradication process usually leads to autoimmune diseases (in the case of insulin, to type 1 diabetes).

Now it should begin to become clear why T cells need MHC. The process of the first contact of a T-cell with an antigen must be controlled, otherwise it may begin to pose a threat to body tissues.
Thus, from a heap of randomly formed T cells, positive and negative selection results in a set of lymphocytes that are able to recognize proteins attached to MHC and safe for their own tissues. After that, these cells are sent to the lymph nodes, where they are activated.
Activation of T-lymphocytes is the process after which these cells become able to actually perform their functions (destroy cells infected with the virus or activate B-cells and macrophages). In the lymph node there is a huge number of dendritic cells that absorb the infectious agent at the site of infection, break it down into proteins and present the corresponding proteins on its surface. After that, if the T-lymphocyte is able to recognize this protein (that is, its receptor is suitable for it), the T-lymphocyte “turns on”. Thus, only those lymphocytes that truly recognize a foreign protein are active.
After activation, T-lymphocytes are able to divide (clonal expansion), and freshly created copies of the lymphocyte in place are activated and enter the bloodstream or move to another area of the lymph node and there are responsible for the activation of B-cells.
B cells
Oddly enough, in general, they are quite similar to T lymphocytes. The main recognition tool, the B-cell receptor, is essentially an antibody attached to the surface of the cell. So let's look at the structure of the antibody.
The basic IgM antibody (immunoglobulin M) consists of two heavy chains and two light chains; each light chain, like the chains of the T cell receptor, consists of a variable and constant region.

The variable region entropy generation mechanism is again similar to the TCR mechanism. There are 40 possible V fragments and 5 possible J fragments, which, if you add a number of random mutations to them, produce a huge number of different possible antibodies.
The fundamental difference between T- and B-lymphocytes lies in the mechanism of selection and activation. B cells do not undergo typical positive and negative selection. To avoid the threat of auto-activity, B-lymphocytes use T-cell selection.
After leaving the bone marrow, B-cells are sent directly to the lymph nodes. On the way, they can capture some proteins with their receptors, absorb them and present them bound to the MHC molecule on their surface.
To activate the B-cell, it is necessary to interact with the T-cell. With this interaction, the T-lymphocyte recognizes the MHC-protein complex on the surface of the B-lymphocyte and, if recognition occurs, activates the B-lymphocyte. It is not difficult to notice that ineffective or autoreactive B cells simply will not be activated, since the T lymphocytes that could do this were removed in the process of negative selection or were not activated.

After activation, the B-cell goes through a process called somatic hypermutation. It begins to divide frequently, and with each division, new mutations are introduced into the region of DNA that encodes the variable region of the antibody. Obviously, B cells that better recognize the antigen will be more frequently and actively activated, and we get ... That's right, normal natural selection. Which ultimately creates B cells, the antibodies of which ideally recognize some kind of antigen.
Ultimately, a B-lymphocyte becomes a plasma cell, which begins to produce antibodies on an industrial scale, and after the threat has passed, it becomes a memory cell that can produce suitable antibodies after a significant period of time.
Thus, the generation of “anti-virus databases” of the human body occurs randomly, however, only those signatures that have shown their effectiveness on pathogens that have already been recognized by heuristic mechanisms become active and are actually used.
The "friend or foe" system. The role of MHC
Unlike macrophages - professional phagocytes that simply devour pathogens, lymphocytes are capable of this, this is not their function. B cells exert their influence by secreting antibodies, and T cells by interacting with other cells.
All T-cells can be divided into three types: T-killets, T-helpers and T-suppressors. I will try to talk about T-suppressors in one of the following parts.
T-killers are designed to destroy pathogens (viruses or bacteria) that are inside the cells. For these purposes, in addition to TCR, they carry adjacent CD8 molecules on the surface, and together TCR and CD8 recognize type I MHC molecules.
MHC I are produced on the surface of every cell in the body. In their absence, the cell is killed by a natural killer (NK cell). All proteins that are inside the cell attach to MHC I. T-killer does not respond to any of them (due to negative selection). However, if a pathogen appears inside the cell, it will also be presented on the surface and will most likely be recognized by the T-killer, and the cell, along with the muck that is inside, will be destroyed.
MHC II is a different case. They are found only on the surface of APC - antigen-presenting cells (these are macrophages, dendritic cells and B cells), and T-helpers recognize them using CD4 molecules similar to CD8.
If proteins that are in the cytoplasm of the cell attach to MHC I, then proteins that were absorbed by the cell from the outside attach to MHC II. Thus, the proteins on the surface of APC are a kind of board “they are being searched for”. T-helpers first activate themselves after contact with a dendritic cell, and then activate B-cells (which begin to produce antibodies) and macrophages (which begin to more actively devour bacteria).

The resulting system is able to recognize the majority of infectious agents, both those that live between cells and intracellular. In addition, she does not spend extra energy on copying obviously inefficient cells and does not attack her own tissues.
Many thanks for the attention and bottomless respect to those who were able to read this heavy text to the end :)
