Keratoectasia (keratoconus, “bulging cornea”): what is it and what to do with it
It happens that a person begins to see into the distance badly, goes to the optics or clinic, finds out that he has myopia or astigmatism (or maybe both at the same time), puts on glasses or lenses that have been written out, use them for some time. Meanwhile, vision continues to deteriorate. The day comes when a person goes to an ophthalmologist at a specialized clinic, sometimes even with the aim of making laser vision correction, and then an unpleasant surprise awaits him: he finds out that he has keratoconus. And it is good if it is latent or early stage of the disease - in this case there is a chance to preserve vision and your own cornea. If this is an advanced process, then we will talk about surgical treatment.
In recent years, patients with keratoconus seem to have become more. But, I think, this is not because someone has started to get sick more often, but because the diagnostic capabilities have improved, and now the conical cornea can be caught in the initial stages.
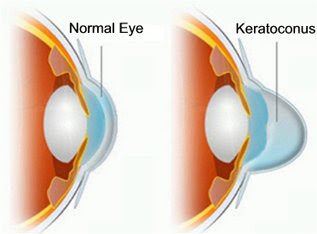
In general, keratoconus is a genetic pathology of the cornea. As the patient grows older, the cornea becomes thinner in the center and is pulled out due to the pressure acting from the inside of the eye. The outer capsule of the eye also loses its elasticity. The first manifestation is abnormal astigmatism. The patient begins to change points frequently, because the axis and the degree of astigmatism change rather quickly.
Where does astigmatism come from? The fact is that the protruding cornea changes the properties of the “lens system” of the eye, and the new “front lens” does not match the projection of the pupil. The cornea with astigmatism is uneven, but regularly-uneven, symmetrical-uneven. When diagnostic scan visible characteristic "butterfly".
More details
The process usually develops in two eyes at different speeds. But, by the way, twins often develop keratoconus at the same time, which confirms the genetic nature of the disease.
Historically, keratoconus was treated by contact, that is, by imposing special lenses that “press back” the cornea and compensate for pressure acting outward. It worked well in the early stages, but as the pathology developed, something more was needed. The next treatment option was end-to-end corneal transplantation, but now there are more interesting procedures, for example, strengthening the cornea tissues due to the combined laser and drug effects, a variety of layered keratoplasty.
It is worth mentioning the sharp form. With the appearance of large cracks in the Descemet's membrane of the eye, acute keratoconus is formed, with it the corneal stroma is saturated with intraocular fluid and becomes cloudy. Visual acuity decreases sharply due to this and related processes. Edema in the center of the cornea may also decrease by itself, without treatment - this is rare, but it happens. In any case, this process ends with an even greater thinning of the cornea.
In addition to genetic (sex-related genes) keratoconus, it is still acquired — most often as a result of injury, but there may be variations (from a surgeon’s error during correction to some rare toxicology), or the disease may develop as a complication of another serious eye pathology. Acquired keratoconus has been little studied, because if we already understand a lot with the lens, there are more or less accurate practical ideas about the retina, even the mechanisms of glaucoma are well studied, but with processes in the cornea there is still much to dig into and what to study. Currently, there is not even a single classification of keratoconus - according to different classifications, the same patient can receive both the first and third stages, since the classifications are based on different indicators. In one clinic they say one thing, in the second - another.
In general, the doctor has two tasks at once: how to stop the development (slow down keratoconus) and what optical method of vision correction for the patient to choose. Depending on the stage and individual characteristics, the necessary type of intervention is selected.
UV crosslinking
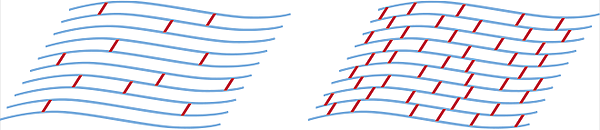
The idea is to saturate the cornea with vitamin B2. By the way, it reacts very well to ultraviolet, so if immediately after that you go above with ultraviolet radiation, then many free oxygen radicals will be released. They will quickly “stick” to the collagen fibers, which will cause the polymerization and “gluing” the fibers together. Let me remind you: in ordinary life, they are intimately fit and slightly bonded, but they form a layered structure in which horizontal bonds are several times stronger than vertical ones. As a result of polymerization, strong horizontal ligaments between the “ropes” of collagen are formed, which leads to cornea hardening. Here is a schematic cross-connection between layers (cross-links) before and after the procedure:
Currently it is the safest procedure for treating keratoconus. Used in the initial and advanced stages, as the lasers improve and diagnostics, the indications for use expand.
UV cross-linking was invented about 10 years ago, and during this time there were quite a few of its modifications and variations, but the general principle of exposure is the same. The eye is saturated with a special solution of riboflavin, then exposure to ultraviolet light, then the formation of new bonds and the withdrawal of other products of riboflavin decay from the eye. The difficulty in determining the required energy level and exposure time - the “gold standard” of the sphere, the so-called Athenian protocol, has now been adopted for the calculation.
In general, the general rule is this: if your ophthalmologist advises UV cross-linking - agree. It is unrealistically difficult to make a mistake when observing the protocol, there are almost no complications. The only thing in many regions of the old school ophthalmologists still say that the cornea is thinner than 400 microns is not affected. Now you can do UV-crosslinking on thinner corneas, just during the procedure a special intermediate contact lens and a slightly different solution of the drug are used.
This is a non-penetrating, rather superficial procedure. Therefore, it carries minimal potential risks. If the instillation mode is not followed, conjunctivitis can be obtained. A couple of examinations are done after the procedure (the first - the next day), the process of corneal epithelization on the contact lens is monitored. A more interesting case is an allergy to solutions and extremely rare toxic reactions. According to subjective sensations, the procedure is unpleasant, for several days until the epithelium of the eyes is completely restored, the tears are present and there is a feeling of “sand” in the eye, a couple of weeks are needed to stop “fogging”.
The second method is the introduction of intrastromal rings (or half-rings)
The logic is very simple: an exogenous skeleton is inserted into the cornea in the form of a ring or a half-ring. It turns out a kind of "corset", which takes on most of the load. Intrastromal corneal rings are perfectly combined with crosslinking, so there are often situations when both are done. The order of operations is very dependent on individual readings, but a bit more often rings are inserted first, then cross-linking is done, since it is better to embed the rings in an elastic medium.

There are various modifications of the intrastromal rings, varying in length, height and configuration. Each manufacturer offers its own nomograms for model selection. There is a good Russian manufacturer who makes them from the same material as imported ones.
Previously, the execution of the tunnels in the cornea was done manually with special lamination and scalpels, now it is done on a femtosecond laser. The operation is performed with micron-precision, as in the ReLEx SMILE, only instead of extracting lenticules, a ring or a semi-ring is inserted into the cavity cut by the laser. Like SMILE, just the opposite. It is done on the same installation (in our case, the 6th generation VisuMAX femtolaser), a separate license is used, which must be obtained by proving to “Zeiss” that the surgeon has such competence. Risks in comparison with a manual operation are much lower, therefore no one has tried to “do it with her hands” for a very long time.
The most unpleasant (at least infrequent) complication is protrusion to the outer canal (when the ring “crawls out”). To avoid this, we make the channels tighter. This requires certain skills of the surgeon, but it can greatly reduce the chances of complications.
More rings can move inside the cornea (most often dumb rotate). This is generally not scary. Sometimes a person begins to torment optical side effects - reflections or "glitches" in the form of highlights in certain lighting. What to do in this case - we decide individually.
The third method is anterior layered keratoplasty
DALK, or anterior deep layered keratoplasty, is the transplantation of the upper layer of the cornea to the Descemet's membrane while preserving the lower layers. That is, the curve of the thinned cornea of the patient is removed to the inner membrane. A transplant is cut out of the cornea of the donor without epithelium, then it is attached. And we together look forward to healing during the year.
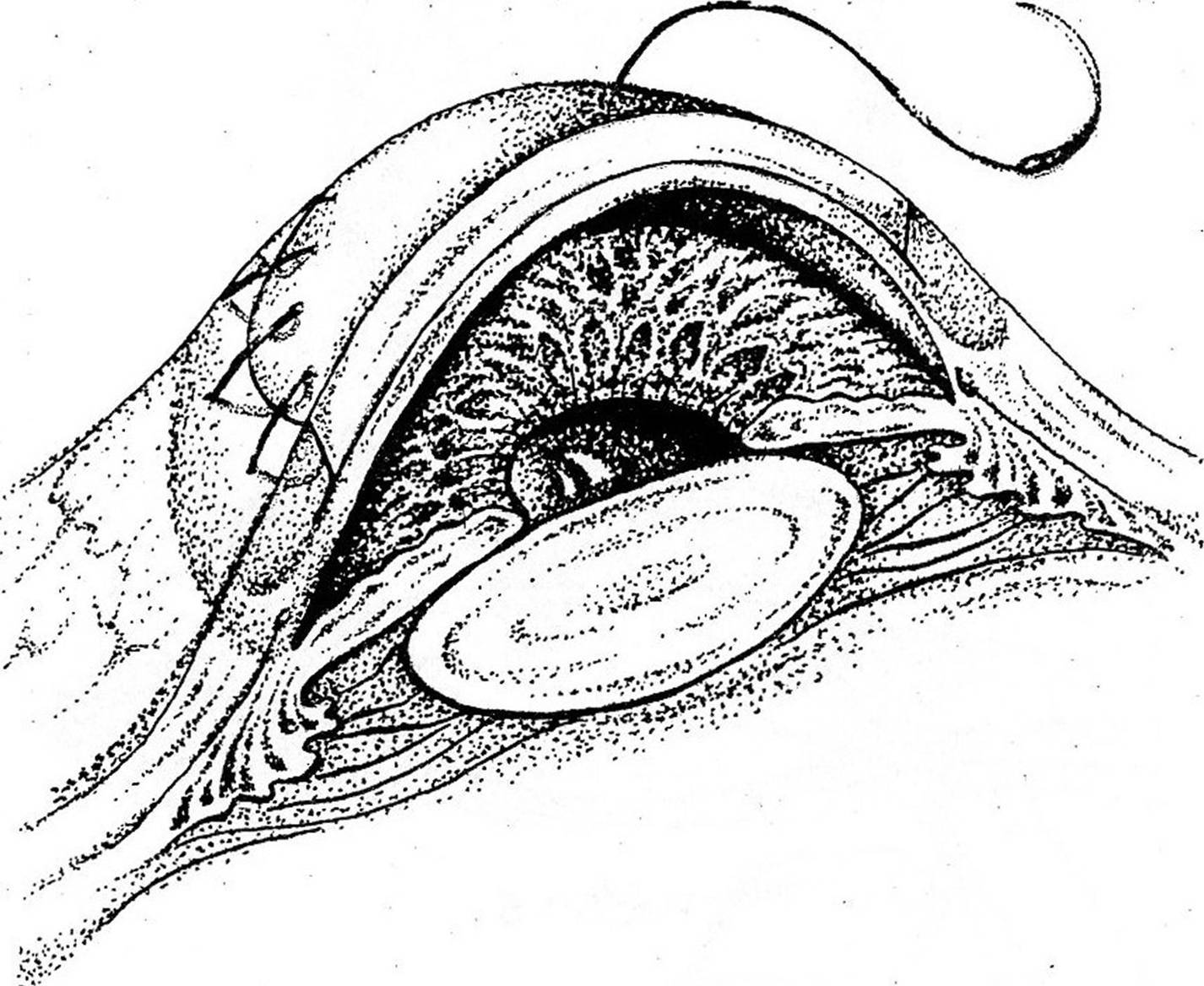
The percentage of survival during keratoconus is quite high (probably the highest among keratoplastic operations) - about 85–90 percent (different sources give different data in this range). This is the most successful transplant - it works well if you have good surgery skills. Often, a femtolaser setup can be used to help the surgeon for more precise cuts.
The method is used when nothing else has helped, or when visual acuity, despite the correction, remains low.
Corneal transplant issues in Russia in recent decades have been painful. While living in the Soviet Union, we actively operated on the cornea, did a lot and well. Then adopted a law on organ donation, when the Union was gone. Legislation in Russia related to the law on transplantation significantly limits the use of corneal transplantation technology. In order to do these operations well, they need to be done a lot and regularly. To do this, always have at hand a sufficient amount of material, it must be available. In Moscow in MNTK them. S.N. Fedorov has an eye bank with a canned cornea, and this allows operations to be performed in a planned manner, and not spontaneously. True, the queue for a transplant is several years - there are a lot of people who want it. In other institutes they use fresh donor one, at the same time as Bulgakov’s: "There is only one freshness - the first, and it is the last." Today, in our clinic, fortunately, there is an opportunity to engage in corneal transplants, not only cross-cutting, but also layering - front and rear. There is access to obtaining corneas of excellent quality (albeit at a very high price). But for patients who suffer from corneal diseases, this is the only chance to get sight. And another plus - the most difficult cases are operated by a professor from Germany, Walter Secundo. He has enormous experience in such operations. They buy donor material from all over the world - fresh from Germany, canned - from the States, Canada and so on. There is access to obtaining corneas of excellent quality (albeit at a very high price). But for patients who suffer from corneal diseases, this is the only chance to get sight. And another plus - the most difficult cases are operated by a professor from Germany, Walter Secundo. He has enormous experience in such operations. They buy donor material from all over the world - fresh from Germany, canned - from the States, Canada and so on. There is access to obtaining corneas of excellent quality (albeit at a very high price). But for patients who suffer from corneal diseases, this is the only chance to get sight. And another plus - the most difficult cases are operated by a professor from Germany, Walter Secundo. He has enormous experience in such operations. They buy donor material from all over the world - fresh from Germany, canned - from the States, Canada and so on.
I must say that I received my experience of layer-by-layer keratoplasty partially in Russia, but mainly in Germany, plus I was lucky with the legislation - I started to operate even when the material was available.
So, we transplant that part of the cornea, which has an average immune reserve. There are a lot of antibodies inside the matrix, and therefore the graft can be rejected. If we compare it with a transplant after inflammation or injury, the situation is still better: the body reacts differently and there are no difficulties with damaged vessels. In general, if transplantation is recommended with optical and at the same time medical purpose, it is necessary to do it. Only with optical - it is better to think a couple of times, world practice - they try to keep their corneas to the limit.
Femtolaser not always used, but it can facilitate one of the stages. The main thing is experienced hands and a lot of practice.
Of the features - during the operation, the transition from the anterior layer-by-layer transplantation to the through-through is possible as the situation in the operating room develops due to the patient's anatomical features (sometimes, the cornea gives perforation intraoperatively). The risk of such a transition depends on the accuracy, patience and experience of the surgeon, and partly on luck.
Relatively often postoperative astigmatism. It is adjusted one and a half years after the removal of sutures.
After cornea strengthening
After the cornea has been strengthened in one of the ways, PRC correction of vision can be done, that is, evaporation of the upper layer with an excimer laser. On a stable cornea with a cone, the operation is possible and it works very well. With PRK, it’s great to level the implanted cornea.
Sometimes we offer implantation of a phakic lens. With patients over the age of 40, we are talking about replacing the lens before a clear indication of cataracts is formed. There are many ways to correct it.
That's about it. The most important thing is that besides simple myopia and astigmatism, which interfere with seeing, but in the future are rather harmless, there is such a serious disease as keratoconus. His presence in the early stages can be detected only by an ophthalmologist with the help of special research methods on complex devices (and even then, if the doctor is competent and is familiar with this problem). It is not enough to check in the optics or clinic. Therefore, with deterioration of vision in the distance and near, frequent change of glasses, the presence of astigmatism and myopia, it makes sense to visit a specialized ophthalmological clinic.
