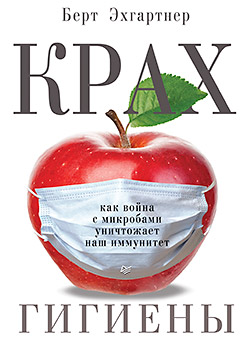
The book “The collapse of hygiene. How the war against germs destroys our immunity. "
 The human body is a huge zoo, and in terms of the diversity of biological species it will not be inferior to the forests of the Amazon. Just imagine: for every human cell in our body there are ten “cohabiting” cells, that is, microorganisms. And they all play their part in a concert of our health.
The human body is a huge zoo, and in terms of the diversity of biological species it will not be inferior to the forests of the Amazon. Just imagine: for every human cell in our body there are ten “cohabiting” cells, that is, microorganisms. And they all play their part in a concert of our health. No one argues that compliance with hygiene principles is one of the most important achievements of civilization. But it seems that the war against microbes has become an end in itself in medicine, and the situation is already out of control. We believed in disinfection, armed with antibiotics and vaccines and destroy viruses and bacteria, not noticing that we are doing irreparable damage to ourselves. Will a man of the 21st century be able to stop the pharmaeddon, which unclean doctors have raised to their banners, and preserve their natural immunity?
Bert Echgartner is an Austrian freelance science journalist, winner of the German Environmental Organization (DUH) award for best journalistic work. In the sphere of his professional interest, health problems and modern medicine invariably turn out to be both official and alternative. In mid-March, a Russian translation of his book is being published at our publishing house.
ALL DISEASES BEGIN IN THE GUT
In addition to the use of antibiotics, many other fundamental issues related to medicine are currently being discussed. It seems that after many years of silence some obstacles in the mental sphere have collapsed. The discovery of the microbiome acted as a catalyst, which allowed us to look at certain phenomena from a new point of view. Hippocrates, the father of modern medicine, wrote 2500 years ago that "all diseases begin in the intestine." Of the hundreds of trillions of microbes that live there, he had no idea, but the fact that he was right in his views was becoming more and more obvious.
Many people advocate for nature and for the conservation of the diversity of species. However, it took a very long time for people to begin to understand that each of us carries biotopes (parts of space inhabited by living organisms) that are also under threat. In the meantime, researchers set up experiments, including on their own, and experiment with various diets, observing their effect on bacteria.
Jeff Leach, a scientist I met recently, lives many months a year in Tanzania, in the savannah, along with a small Hadza people to explore how a person’s microbiome will change if he lives like in the Stone Age. The lich himself is the object of his own experiment - he lives like a Hadza, hunts with them, eats the same prey as they, honey and berries, and for dessert - fat insect larvae. He even started smoking again, since Hadza has the custom of sitting in the evenings together and smoking certain herbs.
Other researchers used themselves and other volunteers as experimental rabbits to study in detail the effects of various antibiotics on the intestinal flora. It turned out that the antibiotic clindamycin has a destructive effect, especially on the groupbacteroids , and dramatically reduces their biological diversity. Bacteroids are among the most important and most numerous species in the colon. But even two years after the course of treatment with antibiotics, their composition did not recover.
Antibiotic ciprofloxacin, which is mainly used to treat urinary tract infections and inflammation of the paranasal sinuses, within three days greatly reduces the variety of species in the intestines. The British researcher Alanna Collen in her interesting book “Silent Power of Microbes” even reports on one study of children in which scientists could not find any bacterial DNA after taking several antibiotics. This means that the microbiome, which many now consider to be its own organ, was completely destroyed in these young children.
INFANTS WITH DIABETES
All these research questions concern urgent problems of our time, such as the huge increase in the number of autoimmune diseases, including type I diabetes, in which the immune system destroys the endocrine cells of the pancreas in the so-called islets of Langerhans. The incidence of type I diabetes in developed countries doubles every 20 years. The most affected age groups are children under five. The daily life of a diabetic is filled with mathematics: you must constantly give yourself injections, measure your blood sugar, weigh each portion of pasta or sauces, convert all carbohydrates to bread units and calculate the appropriate amount of insulin.
Parents of diabetic children do not have a night to sleep. They should wake up late at night, measure their blood sugar to prevent them from exceeding their sugar level or something even more dangerous. If diabetics mistakenly receive excessive amounts of insulin, they are at risk of “hypo” (hypoglycemia), that is, a sharp drop in sugar, which can lead to loss of consciousness and coma - the so-called hypoglycemic shock . Numerous studies show that “hypo” conditions dramatically increase the risk of developing senile dementia, since the brain is very sensitive to periods of hypoglycemia.
The cause of type I diabetes is the "loose" immune system that attacks your own body. But why is the immune system going crazy? Maybe because the body has lost beneficial bacteria? Or did too few regulatory T cells form and the relationships were limited, but we still don’t know about it? The microbes that live in us together have about 20 million genes through which they interfere with the body. So it takes a lot of work to understand even the most important connections.
The reason for Jeff Lich's own experiment was the illness of his daughter, who has been suffering from this auto-aggressive form of diabetes since she was three years old. Jeff is an anthropologist with a degree from the London Higher School of Hygiene. Due to his daughter’s illness, his attitude to the profession changed, and he made the object of his research activities the fascinating world of microbes. “Something in our Western way of life is completely out of control - with our medicine, our nutrition, and our immune functions,” Leach said during one of our conversations on Skype from the savannah with me via satellite . “In my work here, living as a Stone Age man, I hope to find answers that I can take home with me.” Home - this is to his daughter, who is currently studying in Canada. “I thought a lot about what we did wrong. Little she was sick a lot and constantly took antibiotics. I often ask myself the question: if I then had my current knowledge, would we do this with her microbiome? ”
COMMUNICATION BETWEEN THE STOMACH AND THE BRAIN
Increasingly, the "MGB axis", indicating a strong connection between the three most important areas in the body, is at the very center of medical research. The abbreviation MGB means "microbiota, intestines, brain" (microbiota, gut, brain), that is, it postulates the connection of the microbiome and intestines, the largest and most important organ of the immune system, with the nervous system and brain. Microbes regulate bowel function and health. There is increasing evidence that they also affect the immune and nervous systems and the distribution of the flow of information in all directions. This happens unnoticed by us while we are healthy. But how is regulation carried out with numerous diseases during which at least temporary inflammatory processes can occur that affect the brain? There is a lot of evidence that here the MGB axis plays a decisive role.
Currently, diseases are studied in different countries, which at first glance are not connected in any way, but can have common roots. These include autism, ADHD (attention deficit hyperactivity disorder), multiple sclerosis, and various mental disorders.
The connection between the brain and the intestines seems absurd at first glance. But it is no accident that in colloquial German the expressions “solution from the gut” or “gut instinct” (sometimes reminiscent of the Russian “smell inside”) are sometimes used. Nowhere in the body, except the brain and spinal cord, is there such an accumulation of nerve cells. A person’s “abdominal brain” contains 500 million nerve cells - approximately the same amount a dog’s brain has. Evolutionarily, the “abdominal brain” is much older than the brain, but it is very similar to it neurochemically, that is, according to cell types, hormones and receptors. The intestine serves the brain and communicates with it. Communication is conducted in both directions - intestinal bacteria also have something to say.
For example, it occurs during the formation of the neurotransmitter serotonin, which plays an important role in various cognitive processes, such as learning, but is also responsible for good mood and restful sleep. 80% of serotonin in our body is produced in the intestines under the supervision and with the help of bacteria.
Along with this, microbes also produce other chemicals necessary for the functioning of the nervous system, in particular water-insoluble lipids of molecular size, the so-called gangliosides. They are used to build the outer membrane (sheath) of nerve cells.
It is possible that antibiotics can affect this sensitive structure, for example by inhibiting the formation of serotonin or gangliosides. “In adults, this effect may be insignificant,” says Martin Blaser, “but for a child whose brain is actively developing, it can cause significant harm. For example, many studies show that autistic children often have abnormal levels of serotonin. ”
Crohn's disease and ulcerative colitis
With these inflammatory bowel diseases, the immune system attacks its own intestines. The reasons for this are unknown. Perhaps the absence of a microbial field destroyed by antibiotics plays a role. However, it is the latter that are used in the treatment of Crohn's disease and ulcerative colitis, along with various new medicines aimed at calming the immune system.
One of the largest studies on this topic has been conducted in Denmark. Over the past thirty years, the prevalence of ulcerative colitis in children under the age of 15 has more than doubled. And outbreaks of Crohn's disease today affect 15 times more children than in the mid-1980s. Thus, there are more than enough reasons to search for possible triggers.
Between 1995 and 2003, 577,000 children were born in Denmark. All drug prescriptions for these children were recorded, as were all cases of inflammatory bowel disease over a period of six years. Such a large sample allowed scientists to investigate rare relationships as well.
In total, over six years, 117 children fell ill with ulcerative colitis and Crohn's disease. On average, they were about three and a half years old when diagnosed. And here again there was a massive correlation with antibiotics, especially in cases of Crohn's disease. The risk of the disease in children who took antibiotics before this diagnosis was three times higher. There was also a clear association with the doses: each excess prescribed course of antibiotics increased the risk by 18%. Children who received antibiotics seven times or more had a seven-fold greater risk of developing intestinal inflammation than children who did not.
These conclusions and figures paint us a picture that deserves the closest attention. “And when was the last time you heard from your doctor that the next prescription of antibiotics carries a risk of developing a child's asthma or Crohn’s disease?” Asks Martin Blazer. The answer is never.
More recently, Blazer attended a conference where similar issues were discussed. “Suddenly a doctor rose who I did not know, and demanded, given all the information received, to introduce a warning in black frame for anti-biotics.”
This is the most rigorous and eye-catching form of warning that can be administered by the governing medical authorities for prescription drugs. It got its name because of the attention-grabbing black frame inside which a warning is written. Such warnings relate, for example, to possible bleeding when using blood thinners, or that this drug should never be used in the presence of cancer, since it can contribute to tumor growth. In the case of Germany, this would be a “red-handed letter” in which pharmacists and various medical departments and agencies transmit important information. A notable symbol - a red hand on the front of the letter - warns physicians exhausted by constant stress from to drop the envelope to the side and leave it unattended. “Such methods seem necessary to convey to the people the severity of the situation,” says Blazer. By "people", he means primarily colleagues who steadfastly ignore his opinion on the use of antibiotics.
ANTIBIOTIC TEST
Most doctors have firmly learned since studying at the university that antibiotics should be used for bacterial infections. Most recently, a young doctor told me that not prescribing antibiotics for inflammation of the tonsils or middle ear was considered, according to his professor, a serious professional mistake. These old training methods are firmly entrenched in the head, and the mere mention of the fact that we are talking about something “bacterial” is an obvious prerequisite for prescribing an antibiotic.
How can one distinguish whether an infection is viral or bacterial?
Medical device manufacturers have eased this task. A child with a temperature comes to the clinic. There is a suspicion of a bacterial infection of the respiratory tract, or inflammation of the middle ear, or appendicitis - immediately in a well-equipped office, the so-called CPR test is taken. CPR, or C-reactive protein, is a marker of inflammation, the value of which increases with an acute bacterial infection much faster than with a viral infection. For analysis, only one drop of blood is required, which is taken by minimal finger puncture. Within a few minutes, a special device displays the measurement result. With infection, the indicator rises to a value of five to ten milligrams per liter.
In this case, the situation for many parents looks depressing. They hold in their hands a sick, temperamental child that causes acute pity, and then comes confirmation of an “objective” test that the child’s body is obviously experiencing severe inflammation. And again, the doctor, based on a scientific technique, is sure of the right decision when prescribing an antibiotic. Even if the parents are critical of antibiotics, in this case, of course, they will take the prescription. A diagnosis of bacterial infection sounds too scary to resist medical advice.
FIRE FIGHTING
But what is this C-reactive protein? C-reactive proteins (CRPs) are produced in the liver and then released into the blood. They got their name in 1930, when their discoverers noticed that proteins attack pneumococci by binding them to the so-called C-polysaccharide and then dissolving them with calcium ions.
CRPs not only bind to bacteria, but also participate in the processing of dead and dying cells. They contact phagocytes and control some other important mechanisms of the nonspecific immune system. As soon as signs of infection develop in the body, the liver secretes a large amount of protein within a few hours. Usually this process is much faster than the development of a febrile state. In short, CRPs are the “firefighters” of our immune system who are actively involved in the cure of the disease.
In children, this process works especially well, and with a number of commonplace infections, the level of C-reactive proteins increases rapidly. However, here the measurement method can play a trick on us. It would seem that if a high level of CRP shows that the immune system is functioning perfectly and is ready to cope with the disease on its own, why prescribe antibiotics?
But this method is not always perfect. So, for example, sometimes very serious meningococcal infections initially cause only a low CRP response.
As a rationale for this test, it is often mentioned that, as a result, fewer antibiotics are prescribed. Rune Aabenhus and his staff from the University of Copenhagen decided to test this and commissioned an independent Cochrane group to study cases in which the CRP test was used for respiratory infections. However, it really turned out that general practitioners who used the test device prescribed 22% less antibiotics than their colleagues who prescribed prescriptions only on the basis of their own experience. At the worst.
Of course, due to the high level of CRP, people are more likely to be hospitalized. But there were no measurable effects of accelerating the healing process in either case. This is not surprising, given that numerous studies have shown: children after respiratory infections recover quickly with and without antibiotics.
WHO FULFILLS PURPOSES?
How patients or their parents willfully respond to medical recommendations, an Austrian study conducted by the Department of Family Medicine at the University of Vienna shows. The project manager, Catherine Hoffman, collaborated with 30 general practitioners who, for at least 2.5 years, documented the results of their CRP tests and the prescribed drugs. CRP values were divided into three groups: at normal levels, antibiotics were prescribed only in 9.2% of cases, with a slightly increased level - in 71.7%, and with a very high level - in 98.7% of cases. Thus, the decision of the doctors depended mainly on what result the device produced.
Their wards, however, were rather restless. Hoffman analyzed how many recipes were actually bought later in pharmacies, and found that in groups with normal test results and limited antibiotic use, not 9.2%, but still 30.8% somehow managed to get a prescription. Most likely, turning to another, more accommodating doctor.
It is interesting that in the opposite case the same phenomenon occurred: 36% of parents whose children turned out to have a high CRP value and were prescribed a prescription did not take antibiotics in the pharmacy.
Based on the numbers of insurance policies, Hoffman checked what the consequences were. “What was especially interesting,” she writes in her report, “was that none of these patients went to the hospital later.” The fact that they did not follow the recommendations of the doctors had no serious consequences.
The influence of parents on the use of antibiotics is truly enormous. One Swedish study conducted a survey of parents about their relationship to infectious diseases. The higher their level of anxiety, the more often they found themselves with the children in the doctor’s office for the purpose of examination, and the more often their children seemed sick to them, even if they had no temperature or other objective reasons for anxiety. And if these parents were also positive about antibiotics, then the doctors accordingly prescribed them much more often.
»More information on the book can be found on the publisher’s website
