Hepatitis C: “affectionate killer”
When we talk about serious infectious diseases that lead to death and are most stigmatized, we usually mean HIV. Among other diseases, hepatitis C is particularly prominent. Most people infected with hepatitis C virus acquire a chronic infection that is asymptomatic and leads to cirrhosis and liver cancer, and subsequently, death. Because of these characteristics, hepatitis C is nicknamed the “gentle killer”.
Hepatitis C and HIV are often referred to together, and this is no coincidence: today they are the most dangerous rapidly spreading infectious diseases. Both of these diseases are transmitted through blood contact; however, hepatitis C infection through sexual contact is much less likely.
A bit of history
S. P. Botkin discovered the infectious nature of some liver diseases in the 19th century: the disease he described today is called hepatitis A; the following is described, respectively, by hepatitis B. After isolating the causative agents of these diseases, it became clear that they are not the only ones; there is hepatitis “neither A nor B”. RNA of the causative agent of this disease - hepatitis C flavivirus - was detected in 1989 in the blood of patients.
In a large number of cases, hepatitis C is asymptomatic, and a person may not suspect about his illness for many years. The laboratory method is the only one that allows you to reliably determine the presence of infection. To determine the presence of infection, an antibody test (Anti-HCV-total) is used, if the result is positive, PCR and genotyping.
Over time, the disease leads to liver fibrosis (the degree of fibrosis can be determined using elastometry). The degree of F0 is the absence of fibrosis, F4 is cirrhosis. Further progression of the disease leads to the inability of the liver to perform its functions (decompensated cirrhosis) and to the development of liver cancer.
Interferon therapy
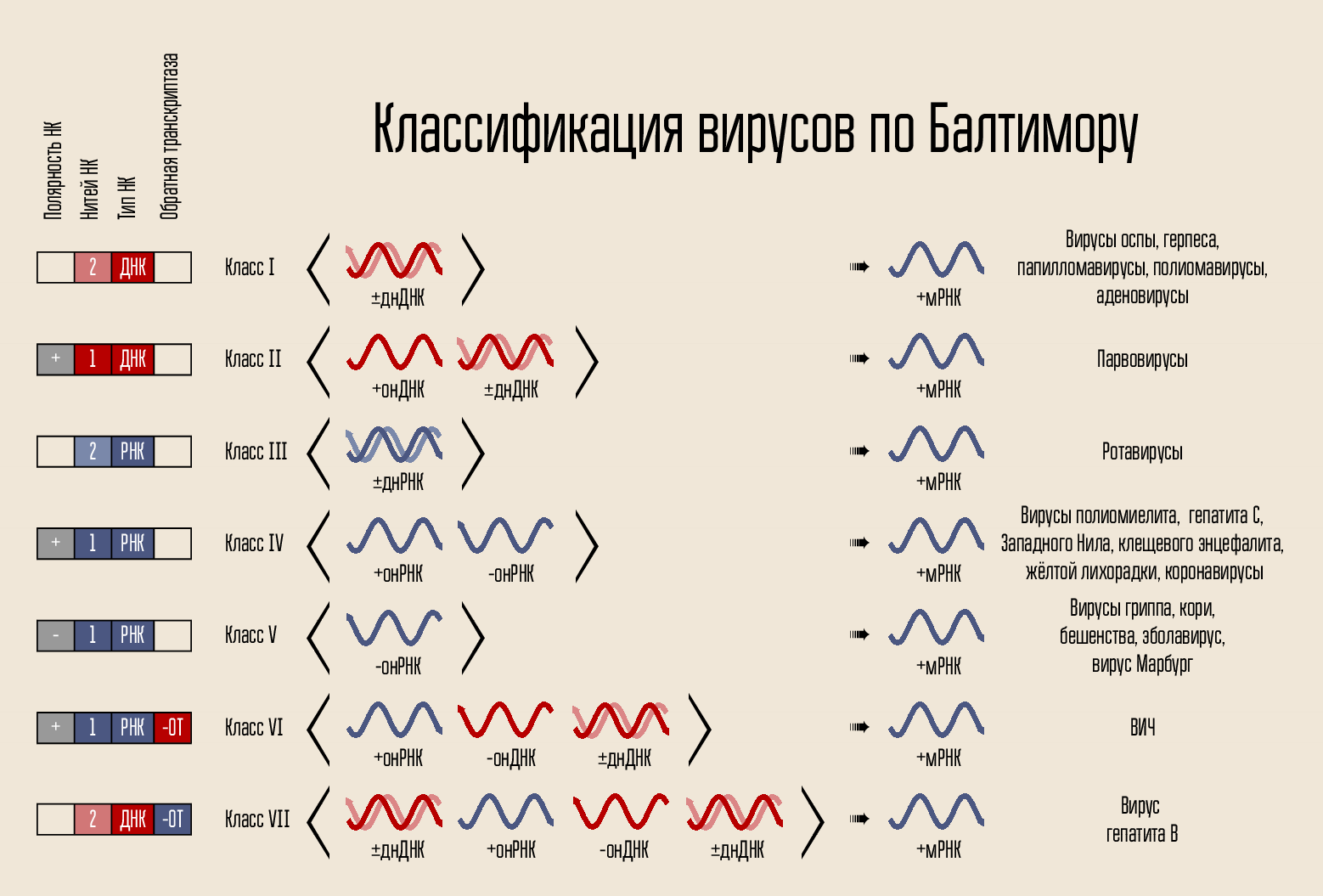
Hepatitis C virus is an RNA-containing virus in the life cycle of which there is no DNA phase. Accordingly, its genetic material cannot be stored indefinitely inside the cell nucleus (as HIV does, for example). This greatly simplifies the approach to treating the disease - if replication of the virus is suppressed for some time, then a complete cure is possible.
The first successful approach to treating the disease was the treatment with interferons (interferon alfa-2a) and ribavirin.
Interferons are proteins that the body produces and which alone do not know how to fight infection. They activate the defense mechanisms in the cells, and that is why the side effects from the use of interferons resemble a flu-like state - the body “believes” that it is sick and begins to fight the infection with the methods available to it. To increase the period of interferon in the body, it binds to polyethylene glycol (pegylation).
Another component of this therapy, ribavirin, is similar to the nucleosides adenosine and guanosine. It consists of sugar (D-ribose) and a part similar to, but not being, a purine nitrogen base. Viral polymerase is trying to build RNA that is complementary to the virus RNA, but it cannot, because it uses ribavirin instead of the desired nucleosides.
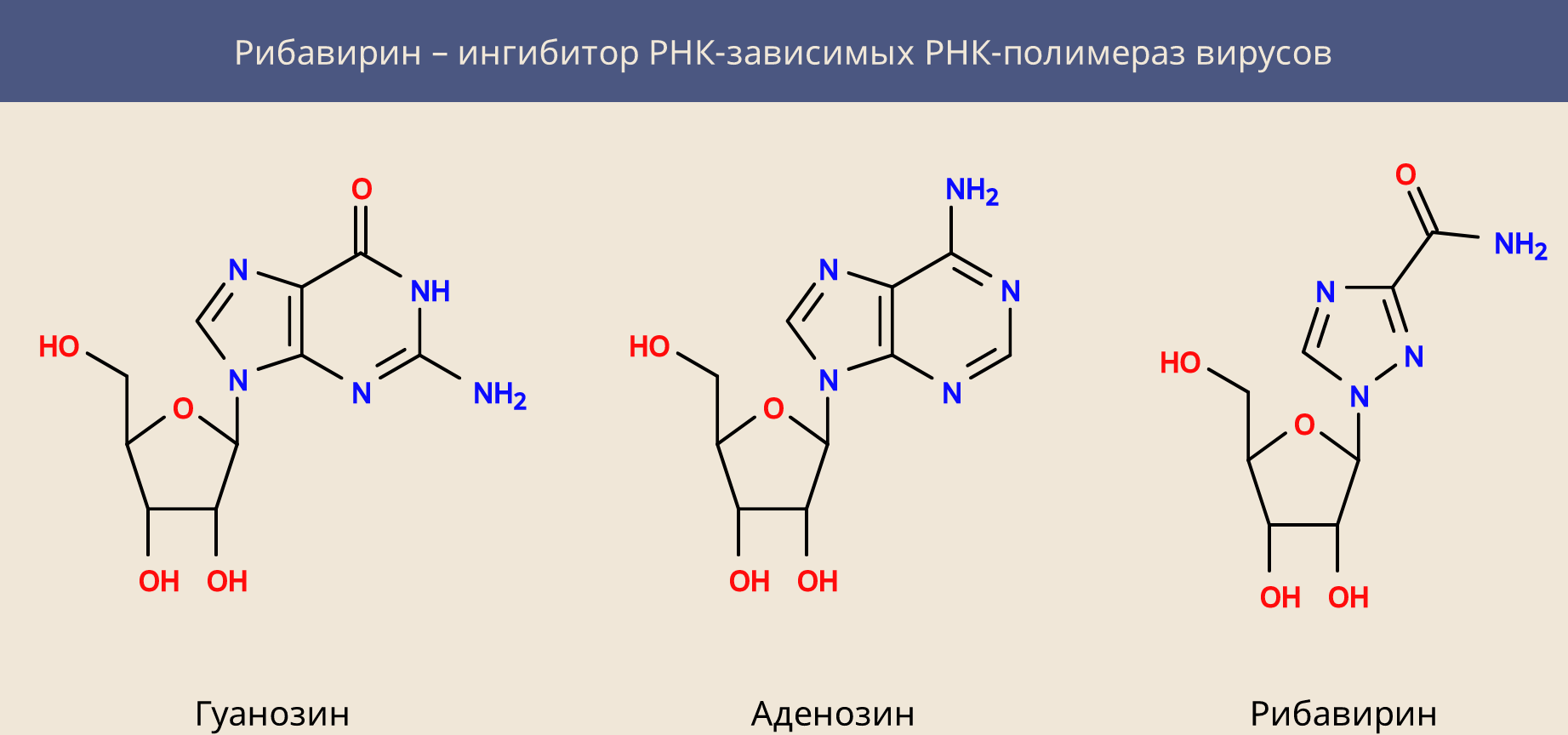
Ribavirin is not a specific cure for hepatitis C, it is active against many other RNA-containing viruses, disrupting the process of rewriting their genome. However, it has another property: it inhibits the cellular dehydrogenase of inosine monophosphate and reduces the intracellular concentration of guanosine triphosphate. This explains both its activity against DNA viruses and its general cytotoxicity.
Interferon-free therapy
Unfortunately, interferon therapy could (depending on the genotype of the virus) cure only 45 to 70 percent of patients. Today, she was replaced by direct, interferon-free therapy.
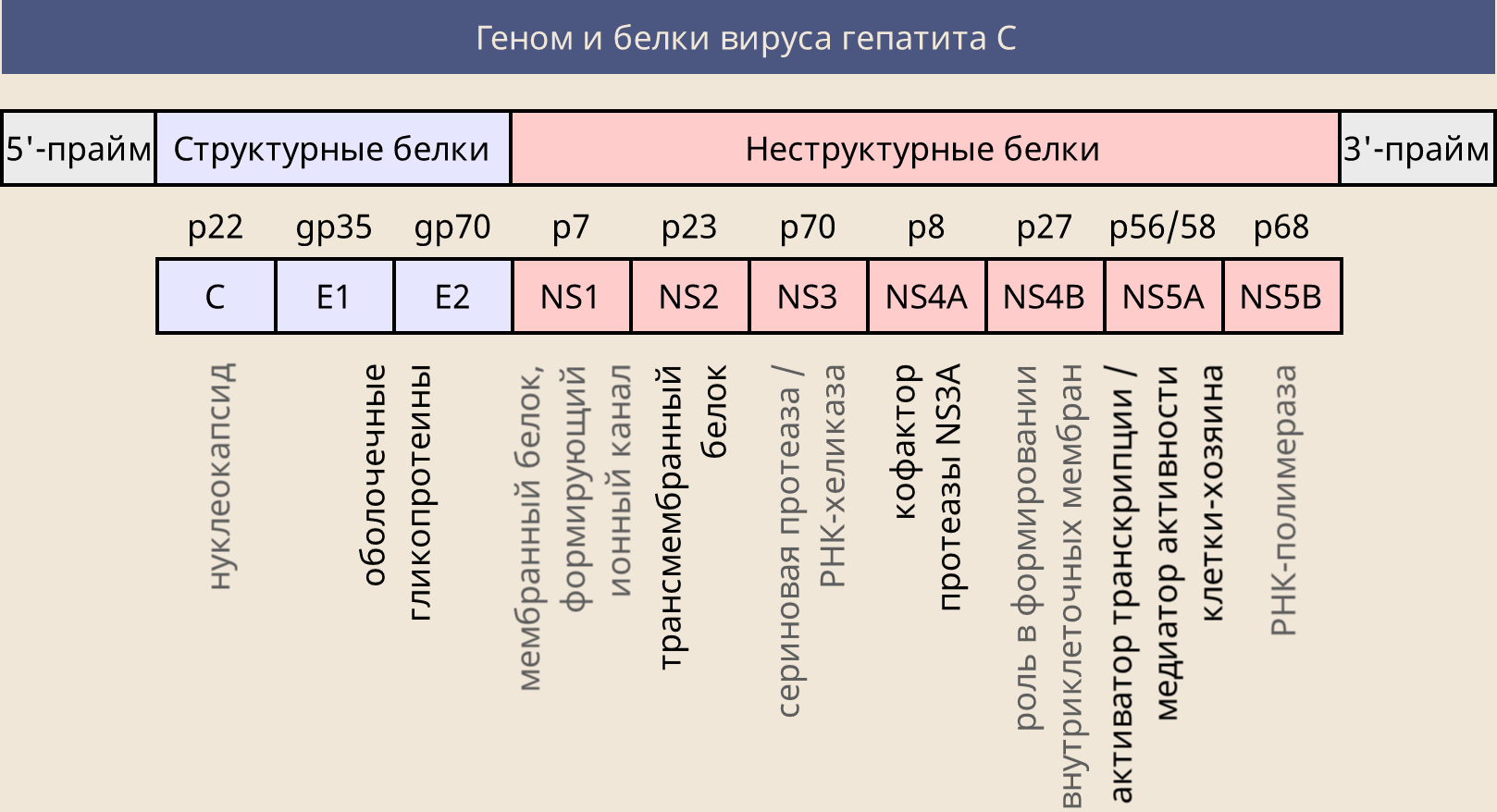
Hepatitis C virus RNA encodes several proteins that the virus needs to complete its life cycle. Among them, structural proteins E1 and E2 (necessary for the assembly of the virus envelope) and non-structural NS (performing certain functions).
The first target of the attack (as for ribavirin) was the NS5B viral polymerase, but this time it was possible to attack it more specifically, creating an analogue of the uridine nucleoside - sofosbuvir. This prodrug, similar in structure to uridine monophosphate, to which additional parts are attached - these parts allow it to freely enter the cell, where, with the help of cellular enzymes, sofosbuvir is converted into the metabolite GS-461203 (triphosphate).
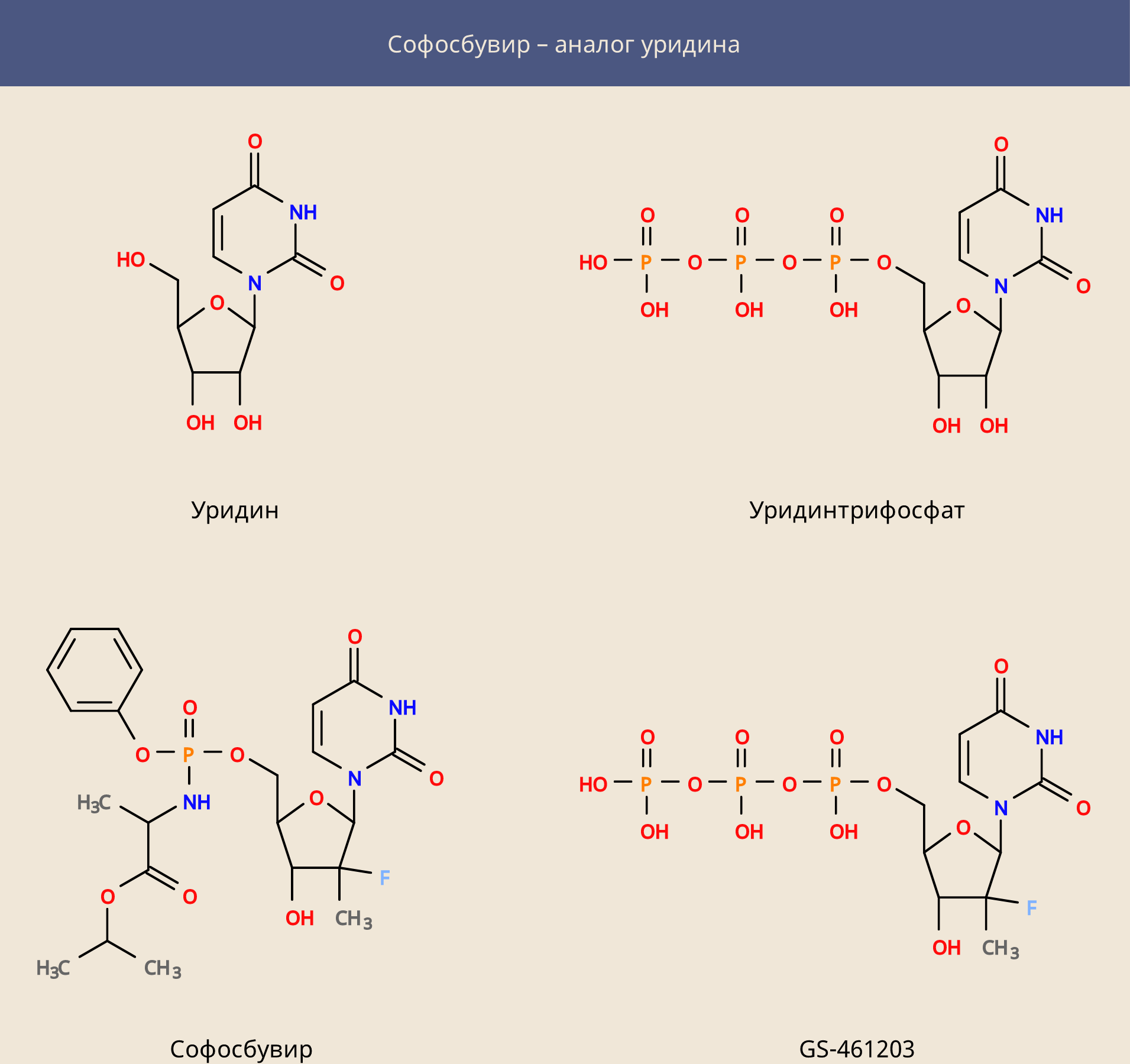
Sofosbuvir itself proved to be an extremely effective medicine, but could not cure all cases of infection. Today, there is a large range of drugs that in most cases can cure hepatitis C.
In addition to the NS5B polymerase, the following are the targets for drugs against hepatitis C virus:
- NS5A protein, which does not have direct enzymatic activity, but plays an important role in the life cycle of the virus (drug names end with -asvir, typical examples are ledipasvir and daclatasvir). Sofosbuvir + Ledipasvir and Sofosbuvir + Daclatasvir are highly effective;
- viral protease NS3 and its cofactor NS4A (drug names end with -previr, for example, simeprevir). According to recent hepatitis C treatment guidelines, the use of protease inhibitors is not recommended for decompensated cirrhosis.
What medicines will not help, and how to choose the right ones?
Only the above types of drugs will help. No hepatoprotectors and folk remedies can help get rid of hepatitis C. The use of interferon-free schemes shows a much higher percentage of cure and fewer side effects, but, for example, in Russia the reality is that the patient in most cases has to take care of buying the medicine himself.
The correct treatment regimen and its duration should be selected exclusively by the infectious disease doctor . It is guided primarily by the degree of liver fibrosis and the genotype of the virus (since the determination of the genotype of the virus can malfunction on recombinant types, the use of pangenotypic drugs is recommended), but not only. An important role is played by the compatibility of drugs with others that the patient is taking, the presence of HIV and / or hepatitis B co-infection, kidney function, and much more.
Unfortunately, there is no vaccine for hepatitis C yet, but the disease is treatable - the main thing is to start therapy on time, before the onset of serious consequences.
